When people think about suicide prevention, they often focus on therapy, crisis support, or medication. These are crucial elements of care, yet the foundations of daily living—sleep, nutrition, and rest—also play an essential role. The relationship between sleep, nutrition, and rest and their impact on suicidal thoughts is often underestimated, but research consistently shows that they influence mood, resilience, and cognitive functioning. By understanding how these basic needs affect mental health, individuals and therapists can create a more holistic approach to healing.
Find a Therapist
Sleep and Suicidal Thoughts
Sleep is one of the most powerful regulators of emotional well-being. Lack of restorative sleep disrupts brain function, decreases impulse control, and amplifies negative thinking patterns. Studies have found strong links between insomnia and suicidal ideation, with those who consistently struggle with sleep reporting higher levels of hopelessness and distress.
From a therapeutic perspective, poor sleep erodes the prefrontal cortex’s ability to regulate emotions, which is why suicidal thoughts often feel more urgent and less manageable after nights of disrupted rest. Cognitive behavioral therapy for insomnia (CBT-I) is one evidence-based approach that helps clients build healthy sleep patterns while addressing anxious or depressive thoughts that interfere with rest. Therapists may also work with clients to reduce nighttime rumination through mindfulness techniques or relaxation exercises.
Improving sleep hygiene is a critical step in suicide prevention. Practices such as establishing a consistent bedtime, reducing screen exposure before sleep, and creating calming routines can strengthen emotional resilience. Therapy can support clients in overcoming the anxiety, trauma, or depression that often underlies disrupted sleep.
Nutrition and Suicidal Thoughts
The saying “food is fuel” applies not only to the body but also to the brain. Nutrition directly influences neurotransmitters such as serotonin and dopamine, which regulate mood. Diets low in essential nutrients—including omega-3 fatty acids, vitamin D, and B vitamins—are linked to higher rates of depression and suicidal ideation. In contrast, balanced nutrition supports cognitive functioning, energy regulation, and emotional stability.
From a therapeutic standpoint, nutrition can be understood through a biopsychosocial lens. Biologically, poor nutrition leads to fatigue and irritability, both of which worsen depressive symptoms. Psychologically, food choices often mirror coping strategies, with individuals turning to high sugar or processed foods to temporarily soothe distress. Socially, cultural or economic barriers may limit access to healthy foods, which can exacerbate health disparities.
Therapists can encourage clients to explore their relationship with food, notice how dietary habits affect mood, and collaborate with dietitians or physicians when necessary. While nutrition alone does not resolve suicidal ideation, it creates a stronger biological foundation for therapy to be effective.
Rest and Its Broader Meaning
Rest is not the same as sleep. It refers to intentional pauses that allow the mind and body to recover throughout the day. In cultures that prioritize constant productivity, rest is often stigmatized as laziness. For people experiencing suicidal ideation, the absence of rest can be devastating because it eliminates opportunities for reflection, emotional regulation, and connection.
Rest can take many forms, including mindfulness practices, gentle yoga, quiet time in nature, or even creative play. These practices reduce activation of the stress response and help regulate the nervous system, making it easier to manage overwhelming thoughts. From the perspective of polyvagal theory, rest activates the parasympathetic nervous system, which counters the hyperarousal that often accompanies suicidal crises.
In therapy, clients often feel guilty for resting. Cognitive behavioral or compassion-focused therapies can reframe rest as a form of survival and self-care rather than indulgence. Rest gives people the capacity to show up more fully in their healing journey.
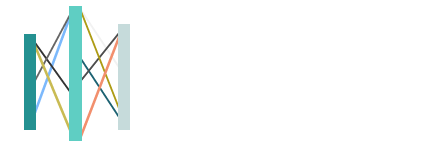
The Interconnection of Sleep, Nutrition, and Rest
Sleep, nutrition, and rest do not function independently. They reinforce one another in complex ways. Poor sleep disrupts appetite-regulating hormones, which contributes to unhealthy eating patterns. Inadequate nutrition worsens sleep and increases fatigue. Without intentional rest, individuals may rely on stimulants or avoidance strategies that create further imbalance.
Therapeutically, this interconnection underscores the value of integrative care. Addressing only one area without the others limits long-term effectiveness. Therapists often explore these domains together, helping clients make small, sustainable changes that strengthen the body and mind’s ability to cope with despair.
Why This Matters for Suicide Prevention
Suicidal thoughts are not caused by poor sleep, nutrition, or rest alone. However, neglecting these foundations weakens coping resources and makes it harder to benefit from therapy or social support. Sleep restores the brain’s capacity for regulation, nutrition fuels resilience, and rest nourishes creativity and reflection. Together, they create a framework where therapy can take deeper root.
By framing these areas as integral to emotional survival, therapists empower clients to view daily self-care not as optional wellness practices but as protective factors against despair. When these foundations are stabilized, clients often report greater hope, clearer thinking, and more energy to engage in therapeutic work.
How Therapists Integrate Sleep, Nutrition, and Rest Into Treatment
While sleep, nutrition, and rest are often discussed as general wellness practices, therapists view them as core components of mental health care. Integrating these foundations into therapy creates a bridge between daily habits and deeper emotional healing, making treatment more comprehensive and sustainable.
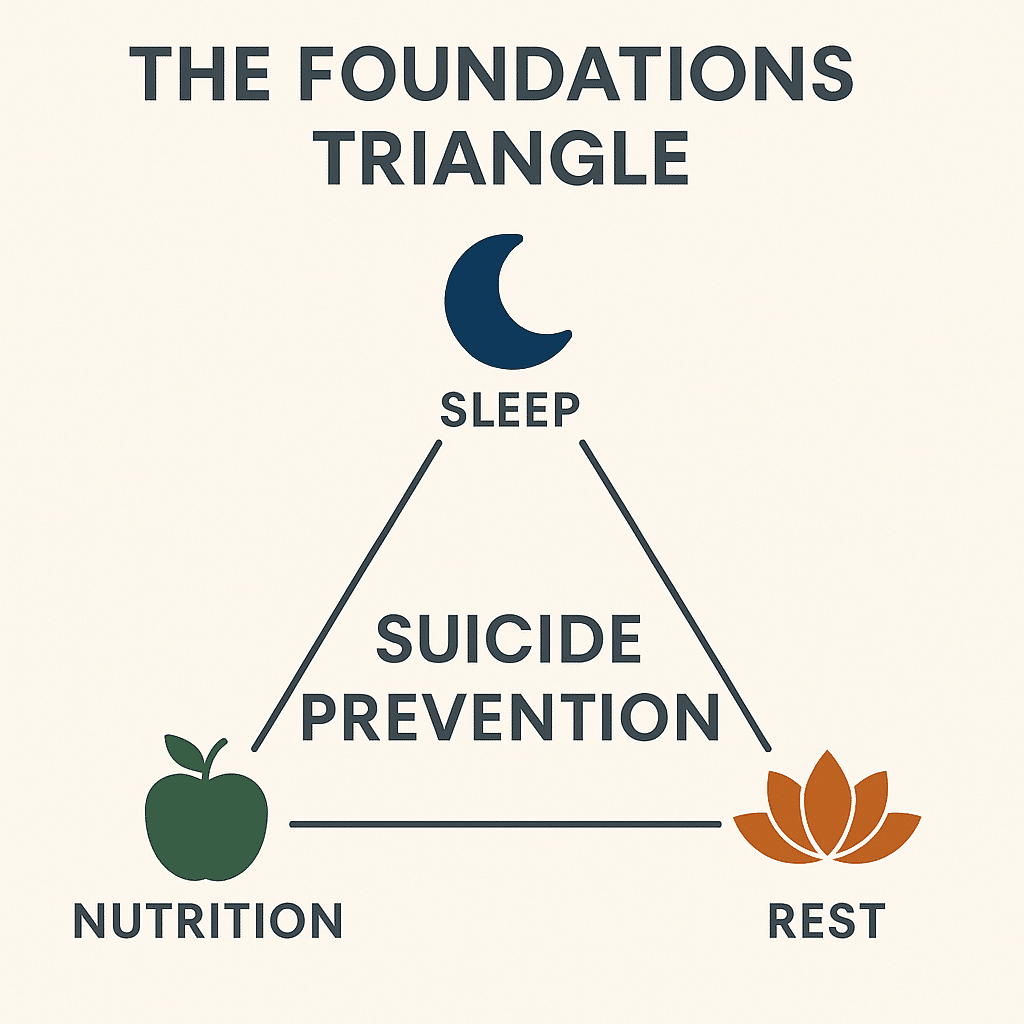
Cognitive Behavioral Therapy (CBT):
In CBT, therapists often help clients track the connections between thoughts, feelings, and behaviors. Sleep and nutrition patterns can be documented and explored to identify cycles that worsen suicidal thoughts. For example, a client might notice that late-night rumination leads to less sleep, which in turn intensifies hopeless thinking the next day. By restructuring unhelpful beliefs and experimenting with new behaviors—such as setting a consistent bedtime routine or balanced meals—CBT helps clients restore both physical regulation and emotional stability.
Dialectical Behavior Therapy (DBT):
DBT emphasizes the role of skills in managing overwhelming emotions, which ties directly into rest practices. Rest can be reframed as a distress tolerance skill, giving clients structured ways to pause, self-soothe, or practice mindfulness. When clients learn to rest intentionally rather than collapse from exhaustion, they gain tools for regulating suicidal urges and finding space between impulse and action.
Polyvagal Theory:
This therapeutic perspective highlights how the nervous system impacts mental health. When people are in a state of chronic stress or sleep deprivation, the nervous system remains activated in survival mode, which increases vulnerability to despair. Rest and consistent nutrition send signals of safety to the body, activating the parasympathetic system and making it easier to access calm states. Therapists can use practices such as breathwork, grounding, or mindful eating to help clients regulate their nervous systems.
Somatic Therapies:
Somatic approaches focus on the mind-body connection and help clients tune into the physical cues of well-being or distress. For example, a therapist might guide a client in noticing how caffeine or sugar impacts mood swings, or how adequate protein leads to a steadier sense of energy and focus. By linking body awareness to choices around sleep, food, and rest, clients build skills for recognizing and responding to their physiological needs before despair escalates.
Integrating these therapeutic approaches shows that sleep, nutrition, and rest are not “extras” but essential building blocks of suicide prevention. By weaving these daily practices into therapy, clients learn to create an internal environment that supports resilience, healing, and hope.
Next Steps
- If you are experiencing suicidal thoughts, immediate help is available through the 988 Suicide and Crisis Lifeline.
- Therapy can help you explore how sleep, nutrition, and rest connect to your emotional well-being.
- Our associate therapists integrate these foundations into their work, creating individualized plans that support resilience and recovery.
- We invite you to browse our therapist directory and connect with a provider who can support you in building a healthier, more balanced foundation for healing.
Find a Therapist
FAQ: Sleep, Nutrition, Rest, and Suicide Prevention
How does sleep deprivation affect the brain’s ability to cope with suicidal thoughts?
Sleep deprivation reduces activity in the prefrontal cortex, which governs impulse control, decision-making, and emotional regulation. This makes it harder to resist suicidal urges and amplifies feelings of hopelessness. From a therapeutic lens, poor sleep creates vulnerability because it weakens the very systems that help people use coping strategies. Restoring sleep is often one of the first steps in building resilience against suicidal ideation.
Why does nutrition play such a strong role in mood regulation?
Nutrition influences the production of neurotransmitters like serotonin and dopamine, which affect mood stability. Deficiencies in essential nutrients are associated with depressive symptoms and higher suicide risk. Balanced diets stabilize energy and improve concentration, which makes it easier to engage with therapy and daily coping strategies. Nutrition, in this way, becomes a supportive foundation for the mind’s ability to heal.
How is rest different from sleep in suicide prevention?
Sleep restores biological functioning, but rest restores psychological and emotional energy. Rest creates intentional moments of pause that lower stress, regulate the nervous system, and provide time for reflection. For individuals struggling with suicidal thoughts, these pauses can act as protective buffers, preventing despair from escalating. Therapists often reframe rest as an active tool for survival rather than a passive luxury.
Can improving sleep, nutrition, and rest replace therapy?
No. While these practices are protective, they do not replace therapy, crisis support, or medical care. Instead, they work in partnership with therapy by stabilizing the body and mind. When individuals sleep better, eat nourishing foods, and allow themselves rest, they arrive to therapy more resourced and able to process painful emotions. The most effective suicide prevention is integrative, blending lifestyle foundations with professional support.
How can therapists address sleep, nutrition, and rest without becoming medical providers?
Therapists can explore how lifestyle factors influence mood, help clients identify barriers, and encourage collaboration with dietitians, physicians, or sleep specialists when needed. They do not prescribe diets or medical plans, but they can validate the connection between basic needs and emotional survival. Many therapeutic models, such as CBT or DBT, already include attention to daily rhythms, making this work a natural part of therapy.
What small steps can clients take to improve sleep, nutrition, and rest?
Small steps may include setting a consistent sleep routine, incorporating one balanced meal daily, or scheduling five minutes of intentional rest. These incremental changes build momentum and reduce the overwhelm that comes with trying to change everything at once. Therapists often emphasize that sustainable progress is more important than perfection.
How do cultural and social factors affect sleep, nutrition, and rest?
Access to nutritious food, safe spaces for rest, and consistent sleep schedules is shaped by culture, environment, and socioeconomic conditions. For example, individuals living in high-stress or unsafe environments may struggle with both sleep and rest. Recognizing these systemic barriers is important so that therapy does not frame these foundations solely as personal failings. Addressing social context helps clients feel validated and reduces shame.
Can rest practices like mindfulness or yoga directly reduce suicidal ideation?
Yes. Rest practices that calm the nervous system help individuals regulate emotions and decrease the intensity of suicidal urges. Mindfulness, yoga, and gentle movement encourage grounding in the present moment, which can disrupt spirals of despair. While they are not cures on their own, these practices give people tools to manage suicidal thoughts more safely until further support can be accessed.
More Reading for Suicide Prevention:
- 10 Books to Explore During Suicide Prevention Month
- Suicide Risk During Major Life Transitions (Divorce, Retirement, Moving)
- When Words Aren’t Enough: Alternative Therapies for Suicide Prevention
- Project Semicolon: An In-Depth Look at Its Origins, Growth, and Mission
- What Project Semicolon Founder Amy Bleuel’s Death Might Teach Us About Suicide
- Understanding Suicide Bereavement: How It Differs from Other Forms of Grief and Effective Therapeutic Approaches
- The Role of Narrative Therapy in Rewriting Suicidal Stories
- Intergenerational Trauma and Its Link To Suicide in Families
- How Attachment Styles Relate to Suicidal Thinking
- 12 Mindfulness Practices for Interrupting Suicidal Thinking
- The Role of Perfectionism and People-Pleasing in Suicidal Ideation
- How Somatic Experiencing Helps Heal Suicidal Despair
- Internal Family Systems (IFS) and the Parts of Us That Want to Give Up
- How DBT Skills Support People Living with Suicidal Ideation
- 10 Ways Art and Music Therapy Serve as Pathways Away from Suicidal Thinking
- 10 Ways Healthy Boundaries Support Suicide Prevention
- Suicide Prevention Through the Lens of Anti-Oppressive Practice
- How Neurodiversity Intersects with Suicide Risk
- 10 Spiritual Practices That Can Help People Facing Suicidal Despair
- Plant Medicine Integration and Transformation After Suicidal Thinking
- 7 Ways Journaling Can Be a Tool for Suicide Prevention