
Living with suicidal ideation is often overwhelming. Thoughts of ending one’s life can feel relentless, leaving little space for hope or relief. For many, these thoughts are not a sign of weakness but a reflection of intense emotional pain and the absence of effective coping strategies. Dialectical Behavior Therapy, better known as DBT, was developed specifically with people in mind who experience persistent suicidal thoughts and self-destructive behaviors. By offering practical tools for regulating emotions, managing distress, and building meaningful connections, DBT skills support people living with suicidal ideation in profound and life-saving ways.
It is important to note that DBT is not a substitute for immediate crisis services. If you or someone you love is in acute danger of acting on suicidal thoughts, contacting the 988 Suicide and Crisis Lifeline or emergency services is the most important step. DBT is a longer-term therapeutic framework that helps people build the resilience and skills needed to reduce suicidal ideation over time.
Find a Therapist
The Origins of DBT
DBT was created by psychologist Dr. Marsha Linehan in the late 1980s. It was originally designed to treat individuals with borderline personality disorder who were experiencing chronic suicidal ideation and self-harm. Over time, DBT has proven effective for a wide range of people who struggle with emotional dysregulation, trauma, and suicidal thinking.
The core philosophy of DBT rests on two principles: acceptance and change. People learn to accept themselves as they are in the present moment, while also working to change patterns that cause suffering. This balance is what makes DBT uniquely effective for individuals caught between the desire to live and the urge to give up.
Why DBT Matters for Suicidal Ideation
Suicidal ideation is often fueled by intense emotional states that feel unbearable. People may experience emotions so overwhelming that escape seems like the only option. DBT acknowledges this reality and provides concrete skills to manage the storm of feelings without resorting to self-harm.
Through structured modules, DBT equips people with tools to:
-
Regulate emotions rather than being consumed by them
-
Tolerate distress without acting impulsively
-
Improve relationships to reduce isolation
-
Stay grounded in the present moment instead of spiraling into hopelessness
These skills directly target the drivers of suicidal ideation, making DBT one of the most evidence-based approaches for suicide prevention.
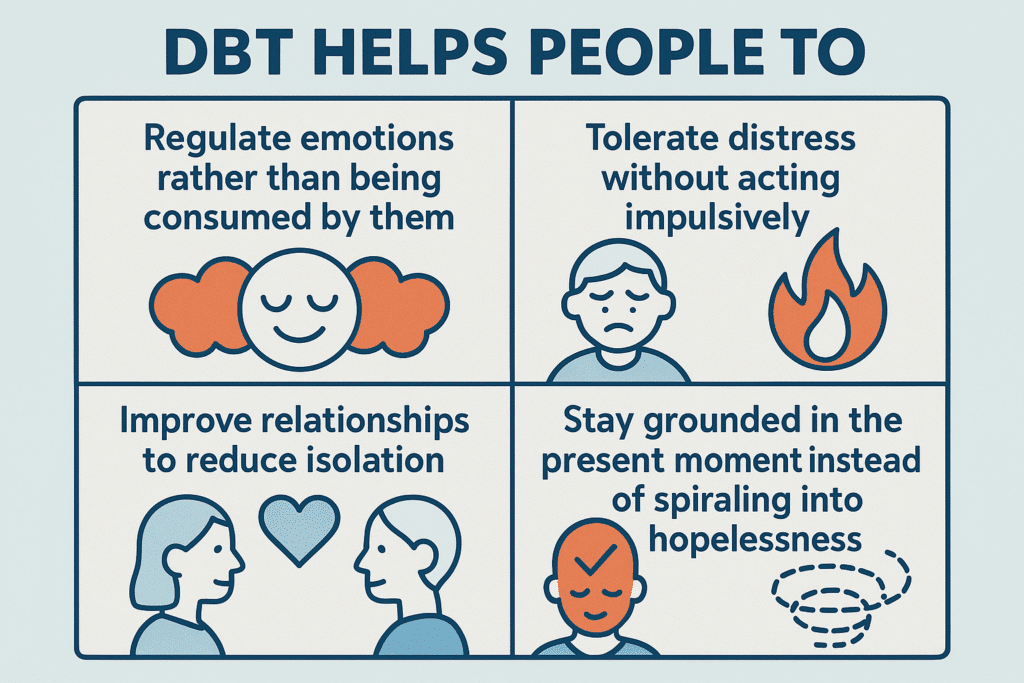
The Four Core DBT Skill Modules
Mindfulness
Mindfulness forms the foundation of DBT. Borrowed from Zen traditions and integrated into behavioral psychology, mindfulness teaches people how to observe their thoughts and emotions without judgment.
How it works: When suicidal ideation arises, mindfulness helps individuals recognize, “I am having the thought that I cannot go on,” rather than fusing with it as an absolute truth. This practice creates a pause, a small space between thought and action. That pause is often life-saving.
Everyday example: Someone struggling with suicidal urges might practice mindful breathing during a lunch break, noticing the rise and fall of their chest. Even a minute of mindful observation can shift attention away from despair and toward the stability of the present moment.
Who it may help most: People whose suicidal thoughts come in intense waves that feel like commands rather than passing mental events.
It might not be for you if: Focusing inward feels unsafe due to trauma. In that case, grounding through external mindfulness, such as noticing sounds or textures in the environment, may be a safer place to start.
Distress Tolerance
Distress tolerance skills are designed for moments of acute crisis. Instead of pushing feelings away or acting impulsively, distress tolerance provides practical tools to survive emotional intensity without self-harm.
How it works: Techniques include sensory grounding (like holding ice cubes), self-soothing with calming scents or sounds, and crisis survival statements such as “this urge will pass.” These strategies do not erase pain but make it bearable long enough for the wave to recede.
Everyday example: A person who feels the urge to overdose might instead submerge their face in cold water for 30 seconds. This shocks the nervous system into the “dive reflex,” slowing the heart rate and reducing emotional intensity, often enough to regain clarity.
Who it may help most: People who experience sudden, overwhelming urges to self-harm or end their lives.
It might not be for you if: You are looking for long-term change. Distress tolerance is designed for survival in the moment, not for healing deeper emotional wounds on its own.
Emotion Regulation
Emotion regulation skills help people understand and manage their emotions rather than being controlled by them. Many people who live with suicidal ideation describe their emotions as chaotic or unmanageable, and DBT directly addresses this.
How it works: Skills include identifying triggers, reducing vulnerability through sleep, nutrition, and exercise, and building positive experiences to balance out despair. Opposite action, one of the core tools, involves acting against destructive impulses, such as calling a friend when the urge is to isolate.
Everyday example: Someone who feels worthless after receiving critical feedback at work might intentionally schedule a pleasant activity, such as a favorite meal or walk, to reduce the spiral of shame and counterbalance negative emotions.
Who it may help most: People whose suicidal ideation is closely tied to mood swings or emotional overwhelm.
It might not be for you if: You are in an immediate crisis. Emotion regulation is powerful but requires practice over time to be effective.
Interpersonal Effectiveness
Isolation and conflict are powerful drivers of suicidal despair. Interpersonal effectiveness skills give people the tools to navigate relationships in ways that foster connection and reduce loneliness.
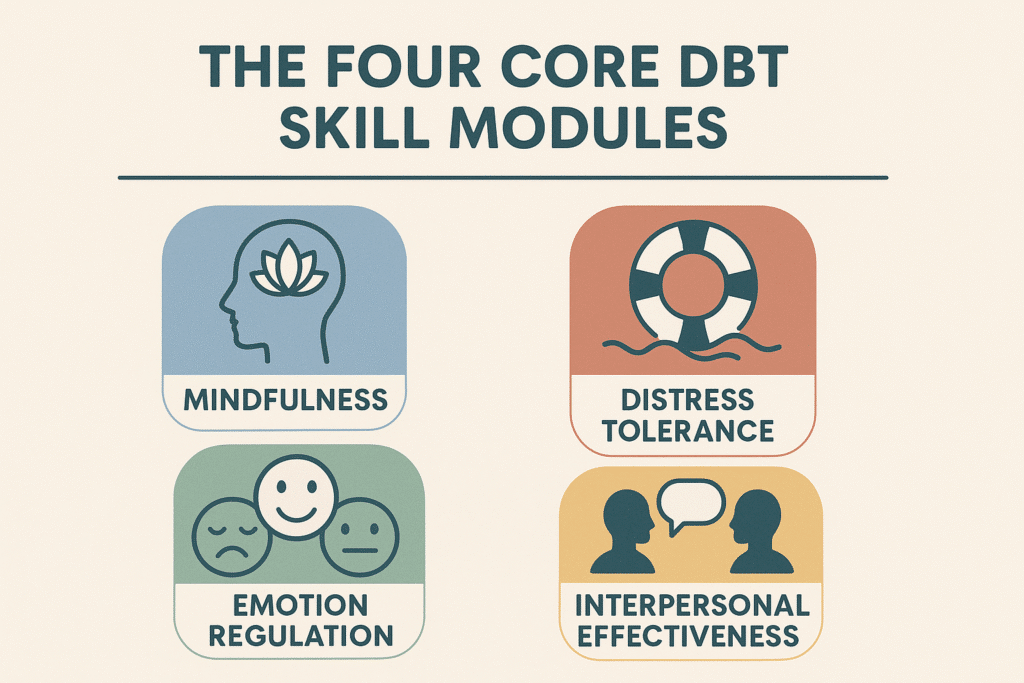
How it works: Skills include DEAR MAN (Describe, Express, Assert, Reinforce, Mindful, Appear confident, Negotiate). For example:
-
-
Describe: State the facts clearly (“I have been struggling lately”).
-
Express: Share your feelings (“I feel alone and overwhelmed”).
-
Assert: Ask directly for what you need (“Could you spend some time with me this week?”).
-
Reinforce: Highlight benefits (“It would mean a lot and help me get through a tough time”).
-
Mindful: Stay focused on the request instead of getting sidetracked.
-
Appear confident: Present your request calmly and firmly, even if you feel nervous inside.
-
Negotiate: Be open to compromise if needed.
-
Everyday example: Someone who feels like a burden to a friend may use DEAR MAN to ask for support without fear of rejection. This reduces isolation and counters the suicidal belief of being unworthy of care.
Who it may help most: People whose suicidal thoughts are rooted in feeling disconnected, rejected, or burdensome.
It might not be for you if: Practicing these skills feels unsafe in abusive relationships. In those situations, safety planning and external supports come first.
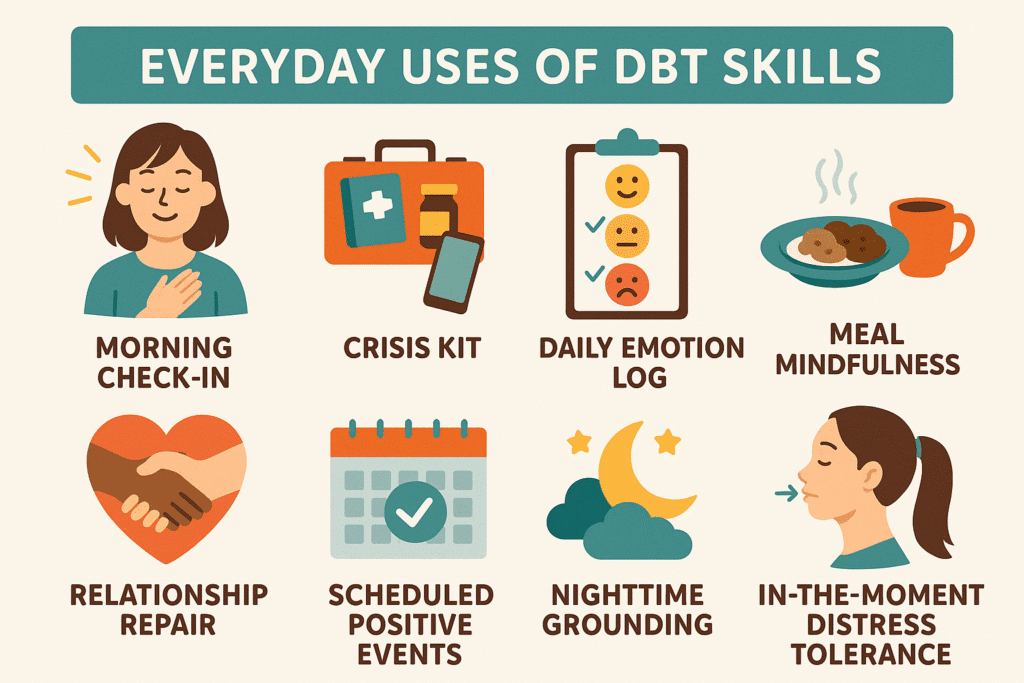
Everyday Uses of DBT Skills
DBT skills are most powerful when woven into daily routines rather than reserved only for moments of crisis. Here are some ways people use them in everyday life:
-
Morning check-in: Beginning the day with three minutes of mindful breathing to set a calm foundation.
-
Crisis kit: Keeping grounding tools such as scented lotion, ice cubes, or soothing music ready to use when urges become overwhelming.
-
Daily emotion log: Writing down emotions throughout the day to track triggers and patterns, then practicing opposite action in response.
-
Meal mindfulness: Eating one meal per day without distractions, focusing on textures, flavors, and gratitude to strengthen mindfulness skills.
-
Relationship repair: Using DEAR MAN after a conflict to express needs and rebuild connection rather than withdrawing in shame.
-
Scheduled positive events: Intentionally planning small joys, like calling a friend, watching a favorite show, or taking a walk, to counterbalance negative emotions.
-
Nighttime grounding: Using a five-senses grounding exercise before bed to reduce racing thoughts and make sleep more accessible.
-
In-the-moment distress tolerance: Carrying a stone, bracelet, or grounding object to touch when urges become strong, anchoring back to the present.
Each practice may feel small, but together they build resilience and create a safety net that makes suicidal thoughts less likely to escalate into actions.
The Structure of DBT
DBT is typically delivered through four interconnected components:
-
Individual therapy: Weekly sessions focused on applying skills to specific challenges.
-
Group skills training: Learning and practicing DBT skills together in a supportive environment.
-
Phone coaching: Real-time therapist support when urges feel overwhelming.
-
Consultation teams: Therapists meet regularly to ensure consistent, effective care.
However, therapists sometimes incorporate DBT techniques with other modalities in standard sessions.
The Role of the Therapist
The therapist plays a central role in making DBT effective. Unlike some therapeutic approaches that focus only on weekly sessions, DBT therapists are actively involved in their clients’ lives through structured support. They provide validation, collaborate on goals, and balance encouragement with accountability.
Therapists help clients:
-
Practice skills in real-life situations, not just in session.
-
Receive coaching between sessions when urges strike, reducing the sense of isolation in crisis.
-
Stay motivated through encouragement while also addressing behaviors that may interfere with progress.
-
Build trust by validating the client’s pain without judgment while still holding hope that change is possible.
-
Navigate setbacks by normalizing relapse and helping clients re-engage with skills rather than sinking into shame.
DBT therapists also model mindfulness, compassion, and nonjudgmental awareness. This relationship itself becomes a stabilizing factor, reminding clients that they are not alone and that they are worthy of care.
Connecting DBT to Suicide Theories
DBT’s effectiveness can be better understood when viewed through established theories of suicide:
-
Psychache theory: DBT provides distress tolerance tools that reduce the unbearable pain Shneidman described.
-
Interpersonal theory: Skills like DEAR MAN address burdensomeness and loneliness described by Joiner.
-
Emotion dysregulation theory: DBT’s emotion regulation skills directly target the overwhelming mood shifts linked to suicidality.
By bridging theory with practice, DBT addresses the root causes of suicidal ideation at multiple levels.
Why DBT Skills Are Life-Saving
The power of DBT is that it meets people exactly where they are. For individuals living with suicidal ideation, this means acknowledging that their pain is real and valid while also believing that change is possible. DBT provides hope not through abstract promises but through concrete tools that can be practiced daily.
Skills such as grounding, self-soothing, and mindful awareness may seem small, but they create the space for life-saving pauses. These moments of pause can make the difference between acting on an urge and surviving to see another day.
Find a Therapist
FAQ: DBT and Suicidal Ideation
DBT is often misunderstood or oversimplified. Below are detailed answers to common questions that go beyond the basics and speak directly to the concerns of people living with suicidal ideation, their loved ones, and those curious about DBT’s unique role in suicide prevention.
How long does it take for DBT to reduce suicidal thoughts?
DBT is a long-term therapy, not a quick solution. Many people notice small shifts within a few weeks, especially with mindfulness and distress tolerance skills that can bring immediate relief in moments of crisis. For example, learning how to ground yourself with sensory exercises or to slow racing thoughts with mindful breathing may reduce the intensity of suicidal urges quickly.
However, meaningful reduction in suicidal ideation typically requires several months of consistent practice. Standard DBT programs run for about a year, with weekly individual therapy, group skills training, and phone coaching. This length of time allows people to not only learn the skills but to apply them repeatedly across different situations until they become second nature. DBT is best thought of as building a toolkit — and like any toolkit, it takes time to assemble and practice using it effectively.
Can DBT be done outside of therapy sessions?
Yes, DBT skills are designed to be portable. Many people practice them independently using workbooks, apps, or online resources. Skills like grounding through the five senses, opposite action, or DEAR MAN can be integrated into daily life without a therapist present.
That said, the full DBT program includes layers of support that make it particularly effective for suicidal ideation. The group setting provides a sense of belonging and accountability, while the therapist offers individualized coaching and crisis support. Without these elements, it is harder to stay consistent, though not impossible. For someone waiting to access therapy, self-practice is a valuable start.
Is DBT only for people with borderline personality disorder?
No. DBT was originally created for borderline personality disorder, but over the past three decades, it has been adapted and tested for a wide range of struggles. It is now widely used for depression, PTSD, eating disorders, substance use, and chronic suicidal thoughts.
The reason DBT is so flexible is because its core skills — mindfulness, distress tolerance, emotion regulation, and interpersonal effectiveness — address problems that many people share, not just those with a particular diagnosis. For example, anyone who feels emotions intensely or has difficulty asking for support may benefit.
How is DBT different from other therapies for suicidality?
Most therapies offer either insight (understanding why we feel the way we do) or techniques (strategies to change how we cope). DBT uniquely balances acceptance with change. It validates that pain is real and overwhelming, while also teaching very concrete skills to survive it.
Compared to CBT, which focuses heavily on thought patterns, DBT incorporates mindfulness and emotional regulation. Compared to psychodynamic therapy, which explores childhood roots, DBT focuses more on practical, here-and-now skills. For suicidality, this is key: DBT does not expect people to eliminate suicidal thoughts overnight but teaches them how to live through the urges safely while gradually reducing their intensity.
What makes DBT particularly effective for suicide prevention?
DBT was one of the first therapies designed specifically for people at high risk of suicide. Its structure ensures people are not left alone in crisis. Phone coaching, for example, means someone can call their therapist outside of sessions when suicidal urges feel unbearable. Group skills training combats isolation by connecting clients with others who understand their struggles.
The philosophy of acceptance and change is also uniquely protective. People with suicidal ideation often feel invalidated — told to “just get over it” or “be positive.” DBT validates that pain is real while also offering concrete hope through change strategies. This dual approach reduces shame, which is a major driver of suicidal despair.
What is the role of the therapist in DBT for suicidality?
DBT therapists are not passive listeners. They are active coaches, teachers, and collaborators. They validate the client’s pain while also challenging harmful behaviors. And they provide real-time coaching to apply skills when suicidal urges strike, ensuring clients feel supported rather than abandoned.
Therapists also help clients track progress, celebrate successes, and learn from setbacks without shame. Importantly, DBT therapists are trained to stay steady even when suicidality feels intense. This stability reassures clients that they are not “too much” or “too broken” to be helped. The therapeutic relationship itself becomes a model of trust and safety, often the first secure connection some clients have experienced.
Can DBT help if suicidal thoughts come from trauma?
Yes. Trauma often leaves the nervous system dysregulated, leading to overwhelming emotional responses. DBT addresses this by teaching grounding and distress tolerance skills for moments of trauma reactivation, as well as emotion regulation skills to stabilize mood over time.
While DBT does not replace trauma processing therapies like EMDR or Somatic Experiencing, it can create the safety and stability necessary before deeper trauma work is possible. In other words, DBT often lays the foundation by giving clients the tools to manage crises that would otherwise derail trauma-focused therapy.
Do DBT skills really work in the middle of a suicidal crisis?
Yes, but they require practice. In the intensity of crisis, it is difficult to learn a new skill for the first time. That is why DBT emphasizes rehearsing skills daily, outside of crisis situations, so they are familiar and accessible when needed.
For example, someone who practices grounding through cold water daily will be more likely to remember and use it when suicidal urges arise. DBT therapists encourage clients to build “distress tolerance kits” with items like scented lotion, grounding stones, or comforting playlists, so they are ready to use in crisis moments.
Can loved ones learn DBT skills too?
Absolutely. Many DBT programs include family education. Loved ones who learn DBT skills can better understand what the person is going through and respond in ways that are validating and supportive rather than dismissive or panicked. For example, instead of saying “don’t think like that,” a family member might say, “I can see you’re in a lot of pain right now, and I’m here with you.”
Family members can also learn to regulate their own emotions, since supporting someone with suicidality can be stressful. This shared language of skills often improves family relationships and reduces conflict.
What if I try DBT and it doesn’t work?
Not every therapy works for everyone, and DBT is no exception. Some people may find group therapy intimidating or struggle with the structured nature of the program. However, even if the full program does not fit, individual skills can still be life-saving. Mindfulness, distress tolerance, and opposite action are useful on their own.
If DBT does not feel effective after a fair trial, it may still open the door to other therapies. Often, clients who start with DBT gain enough stability to engage in trauma-focused work, narrative therapy, or other modalities that address deeper wounds.
Is DBT available online?
Yes. Since the COVID-19 pandemic, many therapists and clinics now offer DBT online, both individually and in groups. Research shows online DBT can be just as effective as in-person, especially when clients stay consistent with attendance and practice. Online DBT also increases access for people who live in areas without specialized therapists.
More Reading for Suicide Prevention:
- 10 Books to Explore During Suicide Prevention Month
- Suicide Risk During Major Life Transitions (Divorce, Retirement, Moving)
- When Words Aren’t Enough: Alternative Therapies for Suicide Prevention
- Project Semicolon: An In-Depth Look at Its Origins, Growth, and Mission
- What Project Semicolon Founder Amy Bleuel’s Death Might Teach Us About Suicide
- Understanding Suicide Bereavement: How It Differs from Other Forms of Grief and Effective Therapeutic Approaches
- The Role of Narrative Therapy in Rewriting Suicidal Stories
- Intergenerational Trauma and Its Link To Suicide in Families
- How Attachment Styles Relate to Suicidal Thinking
- 12 Mindfulness Practices for Interrupting Suicidal Thinking
- The Role of Perfectionism and People-Pleasing in Suicidal Ideation
- How Somatic Experiencing Helps Heal Suicidal Despair
- Internal Family Systems (IFS) and the Parts of Us That Want to Give Up