Reviewed by Kathryn Vercillo, MA Psychology | Last Updated: December 2025
What Are Cognitive and Behavioral Therapies?
Cognitive and behavioral therapies are a family of evidence based psychotherapies that address the connections between thoughts, emotions, and behaviors. These approaches share a foundation in scientific research and practical skill building while offering different emphases to match diverse client needs.
Finding the Right Approach for Your Mind
The way you think shapes how you feel and what you do. This insight, confirmed by decades of research, underlies an entire family of therapeutic approaches that have helped millions of people overcome depression, anxiety, trauma, and other challenges. Cognitive and behavioral therapies offer some of the most extensively studied and effective treatments in mental health.
At Center for Mindful Therapy, our Associate Marriage and Family Therapists throughout the San Francisco Bay Area offer multiple cognitive and behavioral approaches. Whether you seek traditional Cognitive Behavioral Therapy (CBT), the emotion regulation skills of Dialectical Behavior Therapy (DBT), or the values based focus of Acceptance and Commitment Therapy (ACT), you can find therapists trained in these methods throughout our collective.
This page provides an overview to help you understand the cognitive and behavioral therapy family and determine which approach might best serve your needs. Each modality has its own detailed service page where you can learn more.
Browse our Therapist Directory
On This Page:
- Shared Foundations of Cognitive Behavioral Approaches
- Cognitive Behavioral Therapy (CBT)
- Dialectical Behavior Therapy (DBT)
- Acceptance and Commitment Therapy (ACT)
- Comparing These Approaches
- Choosing the Right Approach for You
- Getting Started
- Frequently Asked Questions
Shared Foundations of Cognitive Behavioral Approaches
Evidence Based Practice
All cognitive and behavioral therapies share a commitment to scientific validation. These are not approaches based solely on theory or tradition but methods that have been tested through rigorous research. Hundreds of randomized controlled trials demonstrate their effectiveness across a wide range of conditions.
This evidence base matters for you as a client. When you engage in cognitive and behavioral therapy, you are receiving treatment that research has shown actually works. You are not the first person trying this approach; you are joining millions who have benefited before you.
Present Focused and Practical
While these therapies acknowledge the importance of past experiences in shaping current patterns, they focus primarily on present difficulties and practical solutions. Rather than extensive exploration of childhood, you learn concrete skills and strategies you can apply immediately to improve your daily life.
This practical orientation appeals to clients who want tangible tools rather than open ended exploration. You leave sessions with homework, exercises, and specific techniques to practice.
Skill Building Emphasis
Cognitive and behavioral therapies teach skills. You do not simply talk about your problems; you learn specific methods for managing thoughts, regulating emotions, changing behaviors, and building the life you want. These skills become permanent resources you carry beyond therapy.
This skill building approach means therapy is empowering rather than dependency creating. The goal is for you to become your own therapist, equipped with tools to handle future challenges independently.
Active Collaboration
These therapies involve active participation. Your therapist serves as a teacher, coach, and collaborator rather than a passive listener. You work together to understand your patterns, develop strategies, and evaluate progress. Homework between sessions extends the work beyond the therapy hour.
Structured Sessions
Cognitive and behavioral therapy sessions typically follow a structure: setting an agenda, reviewing homework, working on specific issues, and assigning new practice. This structure ensures productive use of time and keeps treatment focused on your goals.
Cognitive Behavioral Therapy (CBT)
The Foundation of the Family
Cognitive Behavioral Therapy is the original and most widely practiced cognitive behavioral approach. Developed by Aaron Beck in the 1960s and 1970s, CBT focuses on identifying and changing unhelpful thought patterns that contribute to emotional distress.
Core Focus
CBT emphasizes the connection between thoughts, feelings, and behaviors. When you experience distress, CBT helps you identify the automatic thoughts driving that distress, evaluate whether those thoughts are accurate and helpful, and develop more balanced ways of thinking.
The approach addresses cognitive distortions, systematic errors in thinking such as catastrophizing, all or nothing thinking, and mind reading that skew perception negatively. By recognizing and correcting these distortions, you change how you feel.
Key Techniques
CBT uses cognitive restructuring to examine and modify thoughts, behavioral experiments to test assumptions, and behavioral activation to increase engagement in positive activities. Exposure therapy, a behavioral technique, helps overcome anxiety and avoidance.
Best Suited For
CBT has particularly strong evidence for depression, anxiety disorders, panic disorder, social anxiety, specific phobias, OCD, PTSD, and insomnia. It works well for people who appreciate structured, logical approaches and want to understand and change their thinking patterns.
A 2025 meta-analysis published in JAMA Internal Medicine examined 67 clinical trials and found that CBT for insomnia produces large improvements in sleep quality even for people managing chronic health conditions like cancer, chronic pain, and cardiovascular disease. The research showed high client satisfaction and very low rates of adverse effects, confirming CBT’s safety and effectiveness across diverse populations.
Learn More
For comprehensive information about CBT, including detailed techniques, conditions treated, and what to expect in sessions, visit our full Cognitive Behavioral Therapy (CBT) service page.
Dialectical Behavior Therapy (DBT)
CBT Evolved for Emotional Intensity
Dialectical Behavior Therapy was developed by Marsha Linehan in the 1980s for people whose emotional intensity made standard CBT insufficient. DBT maintains CBT’s practical, skill based approach while adding acceptance strategies and specific skills for emotion regulation.
Core Focus
DBT balances change and acceptance through what Linehan calls “dialectics.” You work to change problematic behaviors while also accepting yourself and your current reality. This balance proves essential for people who feel invalidated by purely change focused approaches.
The therapy specifically targets emotional dysregulation, the experience of emotions as overwhelming, rapidly shifting, and difficult to manage. DBT provides skills to tolerate distress, regulate emotions, improve relationships, and stay mindful.
Key Techniques
DBT teaches four skill modules: mindfulness (present moment awareness), distress tolerance (surviving crisis without making things worse), emotion regulation (understanding and managing emotions), and interpersonal effectiveness (asking for what you need while maintaining relationships).
Comprehensive DBT includes individual therapy, skills training groups, phone coaching, and therapist consultation teams. Some clients receive DBT informed individual therapy without all components.
Best Suited For
DBT was originally developed for borderline personality disorder and remains the most effective treatment for this condition. It also helps with chronic suicidality, self harm, eating disorders, substance use, and any presentation involving emotional dysregulation. DBT suits people whose emotions feel overwhelming and who have not found sufficient relief from standard CBT.
Learn More
For comprehensive information about DBT, including the four skill modules, treatment structure, and conditions treated, visit our full Dialectical Behavior Therapy (DBT) service page.
Acceptance and Commitment Therapy (ACT)
A Different Relationship with Thoughts
Acceptance and Commitment Therapy, developed by Steven Hayes in the 1980s and 1990s, takes a different approach to difficult thoughts and feelings than traditional CBT. Rather than trying to change or eliminate negative thoughts, ACT focuses on changing your relationship to those thoughts.
Core Focus
ACT aims to increase psychological flexibility, your ability to be present, open to experience, and engaged in values based action regardless of what thoughts or feelings arise. The goal is not feeling better but living better according to what matters most to you.
Central to ACT is the concept of cognitive defusion, learning to see thoughts as just thoughts rather than facts that must control your behavior. Instead of fighting with difficult thoughts, you learn to let them be present while still taking meaningful action.
Key Techniques
ACT works with six core processes: acceptance (allowing difficult experiences), cognitive defusion (unhooking from thoughts), present moment awareness (mindful contact with now), self as context (the observing self), values clarification (identifying what matters), and committed action (taking steps aligned with values).
These processes work together to help you stop struggling with internal experiences and start building a meaningful life.
Best Suited For
ACT has strong evidence for anxiety, depression, chronic pain, substance use, and stress related conditions. It particularly suits people interested in values based living, those who have tried to control or eliminate difficult thoughts without success, and those drawn to mindfulness and acceptance approaches.
Learn More
For comprehensive information about ACT, including the six core processes, how it differs from CBT, and conditions treated, visit our full Acceptance and Commitment Therapy (ACT) service page.
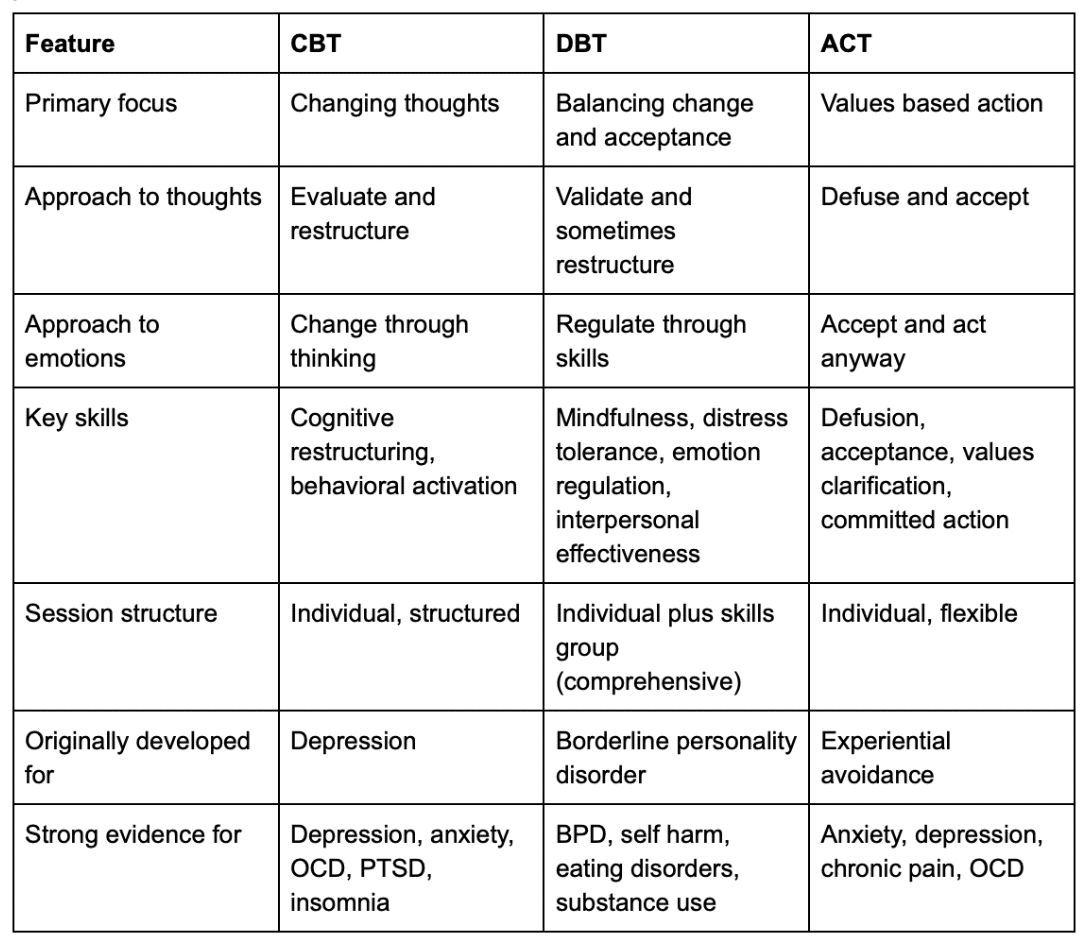
Comparing These Approaches
Research published in the Psychiatric Clinics of North America confirms that CBT, DBT, ACT, and mindfulness based approaches all belong to the same family of effective treatments, each offering unique strengths while sharing core therapeutic principles. Meta-analytic findings show these approaches produce moderate to large improvements in anxiety and depression across varied populations.
Approach to Thoughts
The three therapies differ most notably in how they work with difficult thoughts.
- CBT examines thoughts to determine their accuracy, then works to change distorted or unhelpful thoughts to more balanced alternatives. The assumption is that more accurate thoughts lead to better emotions.
- DBT includes cognitive restructuring like CBT but adds radical acceptance. Some thoughts and situations cannot be changed and require acceptance rather than modification. DBT balances changing what you can with accepting what you cannot.
- ACT does not try to change thought content. Instead, you change your relationship to thoughts through defusion, seeing thoughts as mental events rather than facts that must control behavior. A thought can be present without determining your actions.
Relationship to Emotions
- CBT views problematic emotions as often resulting from distorted thoughts. Change the thought, change the emotion. Emotions serve as signals that thinking may need examination.
- DBT validates emotions as understandable given history and biology. Rather than immediately trying to change emotions, you learn to tolerate distress and regulate emotions skillfully. Emotions are not problems but experiences requiring management skills.
- ACT encourages acceptance of all emotions as part of human experience. Rather than trying to feel differently, you learn to take valued action regardless of emotional state. Emotions are allowed rather than controlled.
Treatment Goals
- CBT aims for symptom reduction through cognitive and behavioral change. Success means less depression, less anxiety, fewer problematic behaviors.
- DBT aims for a life worth living through building skills and reducing life threatening and therapy interfering behaviors. Success means stable emotion regulation, effective relationships, and engagement with valued activities.
- ACT aims for psychological flexibility and values based living. Success means living meaningfully according to your values regardless of internal experiences. Symptom reduction often occurs but is not the primary target.
Choosing the Right Approach for You
Consider Your Primary Concerns
Different cognitive behavioral approaches excel with different issues. If you struggle primarily with depression, anxiety, or specific phobias, traditional CBT has the longest track record. If emotional intensity, self harm, or relationship chaos are central concerns, DBT offers specialized skills. If you feel stuck fighting against your own thoughts and want to focus on building a meaningful life, ACT provides a different framework.
Consider Your Preferences
Your personal preferences matter. Some people appreciate CBT’s logical, analytical approach to examining thoughts. Others feel more drawn to DBT’s validation and acceptance emphasis. Still others resonate with ACT’s focus on values and meaning.
Consider: Do you want to analyze and change your thoughts (CBT)? Learn skills for managing overwhelming emotions (DBT)? Stop struggling with thoughts and focus on values based living (ACT)?
Consider What You Have Already Tried
If you have tried traditional CBT and found the focus on changing thoughts insufficient, DBT or ACT might offer what was missing. If you have tried acceptance based approaches but need more cognitive structure, CBT might be better. Your history with different approaches provides useful information.
You Do Not Have to Choose Alone
Many of our therapists have training in multiple cognitive behavioral approaches and can help you determine which best fits your needs. Some integrate elements from different approaches based on what serves each client. A consultation can help clarify which direction makes sense for you.
These Approaches Are Not Mutually Exclusive
You might begin with one approach and add elements of another as treatment progresses. Someone might start with DBT skills to stabilize emotional regulation, then incorporate CBT cognitive restructuring, then move toward ACT values work. Your therapist can guide you through what serves you best at each stage.
Getting Started
Explore the Detailed Service Pages
Each therapy has its own comprehensive service page with detailed information about techniques, conditions treated, session structure, and what to expect. We encourage you to read the pages that interest you:
- Cognitive Behavioral Therapy (CBT): The foundational approach focusing on thought restructuring and behavioral change
- Dialectical Behavior Therapy (DBT): Skills based therapy balancing change and acceptance for emotional intensity
- Acceptance and Commitment Therapy (ACT): Values based therapy focusing on psychological flexibility
Browse Our Therapist Directory
Our directory allows you to filter by therapeutic approach. Look for therapists who list CBT, DBT, or ACT among their modalities. Read profiles to understand each therapist’s specific training and approach within these frameworks.
Some therapists specialize primarily in one approach. Others integrate multiple cognitive behavioral methods. Consider whether you want a specialist or a generalist based on your needs.
Schedule a Consultation
If you remain unsure which approach fits best, schedule consultations with therapists who use different methods. Many offer brief phone consultations before committing to a first session. These conversations can help clarify which approach resonates with you.
In Person and Telehealth Options
Our therapists offer cognitive and behavioral therapies both in person throughout the San Francisco Bay Area and via telehealth throughout California. All three approaches translate effectively to video sessions, allowing you to access specialized care regardless of location.
Browse our Therapist Directory
For questions or help finding the right therapist, contact us.
Frequently Asked Questions
Q: Can I receive more than one type of cognitive behavioral therapy at the same time?
A: Yes, many therapists integrate elements from multiple cognitive behavioral approaches based on client needs. You might work on cognitive restructuring (CBT) while also learning distress tolerance skills (DBT) and clarifying values (ACT). Skilled therapists draw from whatever serves you best rather than rigidly adhering to a single protocol.
Some clients work with two different therapists simultaneously, perhaps receiving individual CBT while attending a separate DBT skills group. If you pursue this approach, ensure your providers communicate so treatment remains coordinated.
The cognitive behavioral approaches share enough common ground that integration is natural. They all emphasize present moment focus, skill building, and active participation. The differences lie more in emphasis and specific techniques than in fundamental incompatibility.
Q: How do I know if I need DBT versus regular CBT?
A: Consider whether emotional intensity is a central part of your struggles. If your emotions feel overwhelming, shift rapidly, or lead to impulsive behaviors you later regret, DBT’s specialized emotion regulation skills may serve you better than standard CBT. DBT was specifically developed for people whose emotional intensity made regular therapy insufficient.
Also consider self harm, suicidal behavior, or chronic relationship chaos. DBT has the strongest evidence for these presentations. If these concerns are prominent, DBT should be seriously considered.
If your primary concerns are more straightforward depression, anxiety, or specific fears without significant emotional dysregulation, standard CBT may be sufficient and has an extensive evidence base for these conditions.
When uncertain, a consultation with a therapist trained in both approaches can help determine which fits your presentation best. Many people benefit from CBT who might also benefit from DBT; the choice often comes down to severity and personal preference.
Q: Is ACT better than CBT because it is newer?
A: Newer does not mean better. Both ACT and traditional CBT have strong research support, and head to head comparisons generally show similar effectiveness for conditions like anxiety and depression. The question is not which is objectively superior but which approach fits you better.
ACT offers a different framework that resonates strongly with some people, particularly those who feel exhausted from fighting with their thoughts or who are drawn to values based living and mindfulness concepts. Traditional CBT appeals to those who appreciate logical analysis and want to directly address distorted thinking.
Some research suggests ACT may have advantages for certain presentations, particularly chronic pain and conditions involving significant experiential avoidance. But CBT has a longer track record and more extensive research for conditions like depression and specific anxiety disorders.
Choose based on what resonates with you rather than assuming newer is automatically better. The best therapy is the one you will engage with fully.
Q: What if I start one approach and realize it is not working?
A: This happens and is not a failure. Different people respond differently to various approaches, and sometimes you need to try something to know whether it fits. A good therapist monitors progress and adjusts treatment when needed.
If after several sessions you feel the approach is not clicking, discuss this openly with your therapist. They may be able to incorporate elements from other cognitive behavioral approaches or refer you to a colleague who specializes in a different method.
Signs an approach may not be working include feeling like the therapist does not understand your experience, finding the techniques unhelpful or forced, or making no progress on your goals after adequate time. Trust your experience while also giving approaches time to work before abandoning them.
Q: Are cognitive behavioral therapies appropriate for trauma?
A: Yes, with important considerations. Trauma focused CBT approaches, including Cognitive Processing Therapy (CPT) and Prolonged Exposure, are highly effective for PTSD. DBT addresses trauma indirectly by building distress tolerance and emotion regulation skills that help survivors manage trauma related activation. ACT helps trauma survivors stop avoiding painful memories and build meaningful lives despite traumatic history.
However, cognitive behavioral approaches are not the only option for trauma. Some trauma survivors benefit from approaches that work more directly with the body and nervous system, such as EMDR or somatic therapies. The best choice depends on your specific presentation, preferences, and what you have already tried.
If trauma is your primary concern, seek a therapist with specific trauma training regardless of their cognitive behavioral orientation. Trauma work requires specialized skills beyond general CBT, DBT, or ACT training.
Q: Can children and teens receive these therapies?
A: All three cognitive behavioral approaches have been adapted for younger clients. CBT has extensive evidence for treating anxiety and depression in children and adolescents. DBT has been modified for teens, particularly those struggling with self harm, suicidal behavior, or emotional dysregulation. ACT has also been adapted for younger populations.
The adaptations account for developmental differences in cognitive ability, attention span, and what engages younger clients. Therapy with children and teens typically involves more activity, games, and creative expression than adult versions. Parent involvement is often part of treatment.
Our therapist directory allows you to filter for therapists who work with children, teens, and families. If you seek cognitive behavioral therapy for a young person, look for therapists with specific training and experience in child and adolescent treatment.
Citations:
- Scott, A. J., Correa, A. B., Bisby, M. A., Chandra, S. S., Rahimi, M., Christina, S., Heriseanu, A. I., & Dear, B. F. (2025). Cognitive behavioral therapy for insomnia in people with chronic disease: A systematic review and meta-analysis. JAMA Internal Medicine, 185(11), 1350–1361. https://doi.org/10.1001/jamainternmed.2025.4610
- Hofmann, S. G., Sawyer, A. T., & Fang, A. (2010). The empirical status of the “new wave” of CBT. Psychiatric Clinics of North America, 33(3), 701–710. https://doi.org/10.1016/j.psc.2010.04.006