Suicide prevention cannot be understood through a single lens. People experience despair differently depending on their identities, histories, and ways of processing the world. Among the most important yet often overlooked perspectives is neurodiversity. Understanding how neurodiversity intersects with suicide risk allows clinicians, families, and communities to better recognize vulnerabilities while also appreciating the unique strengths and needs of neurodivergent individuals.
Find a Therapist
What Is Neurodiversity?
The term “neurodiversity” was coined in the late 1990s to describe the natural variations in human brains and minds. Instead of framing conditions such as autism, ADHD, dyslexia, or other developmental differences solely as deficits, neurodiversity emphasizes that these are part of the spectrum of human diversity. Neurodivergence does not inherently cause suffering, but stigma, lack of accommodation, and misunderstanding often do.
For many people, embracing neurodiversity means affirming identity and fostering belonging. However, it is equally important to acknowledge the mental health challenges that can accompany being misunderstood, marginalized, or unsupported. Suicide risk among neurodivergent individuals is one such challenge.
Suicide Risk Among Neurodivergent Populations
Research highlights that neurodivergent individuals experience disproportionately high rates of suicidal thoughts and behaviors compared to the general population. For example, studies consistently show that autistic individuals are significantly more likely to experience suicidal ideation, with some estimates suggesting rates more than three times higher than those of neurotypical peers. People with ADHD also demonstrate elevated suicide risk, often linked to impulsivity, co-occurring conditions, and challenges with emotional regulation.
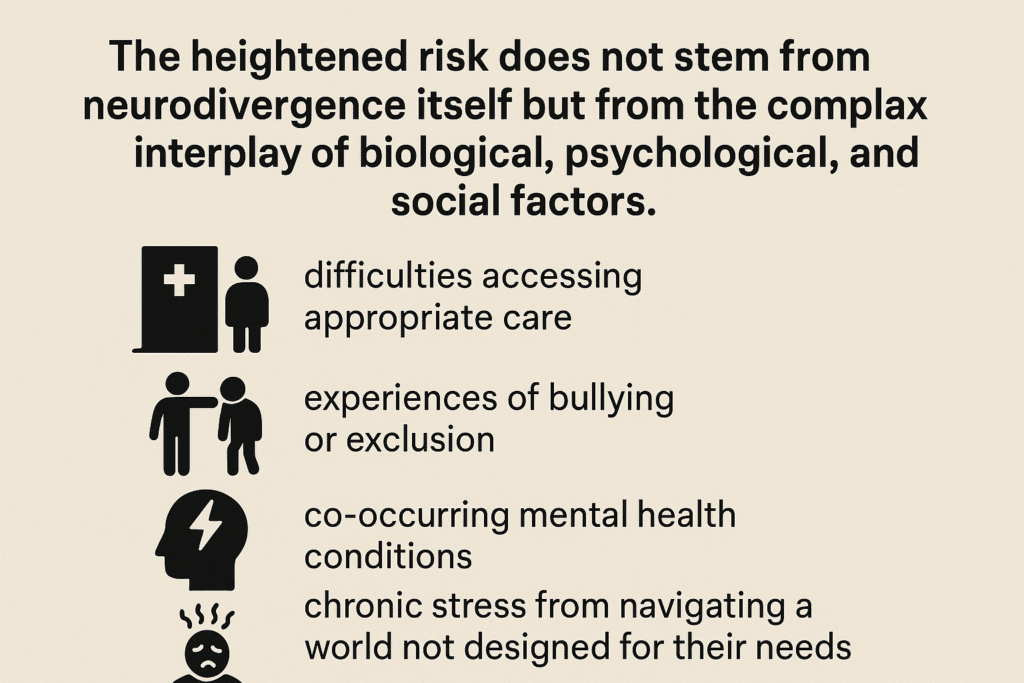
The heightened risk does not stem from neurodivergence itself but from the complex interplay of biological, psychological, and social factors. These include difficulties accessing appropriate care, experiences of bullying or exclusion, co-occurring mental health conditions, and chronic stress from navigating a world not designed for their needs.
The Role of Stigma and Isolation
One of the most profound contributors to suicide risk in neurodivergent populations is social stigma. Being misunderstood, dismissed, or ridiculed can lead to profound feelings of isolation. For autistic individuals, for instance, sensory differences or social communication challenges may result in exclusion or bullying. People with ADHD may internalize repeated criticism about their focus, organization, or behavior.
Over time, this accumulation of negative experiences erodes self-esteem and contributes to hopelessness. When neurodivergent individuals feel that they cannot belong or succeed within societal expectations, suicidal ideation may emerge as an expression of despair.
Emotional Regulation and Co-Occurring Conditions
Another factor in how neurodiversity intersects with suicide risk involves emotional regulation. Many neurodivergent individuals experience heightened sensitivity to stress or difficulty managing strong emotions. When combined with co-occurring conditions such as anxiety, depression, or trauma, the risk for suicidal ideation increases.
For those with ADHD, impulsivity can intensify risk, as suicidal thoughts may be acted upon more quickly. For autistic individuals, challenges with communication may make it harder to express distress or to seek help, leaving pain unrecognized until it reaches a crisis point.
Barriers to Mental Health Support
Accessing appropriate care is often more difficult for neurodivergent individuals. Traditional talk therapy may not always meet their needs if clinicians are not trained in neurodiversity-affirming approaches. Misdiagnosis or misunderstanding can further complicate care, as symptoms of neurodivergence may be mistaken for unrelated disorders.
This gap in care contributes directly to suicide risk. When individuals feel invalidated or unsupported in mental health settings, they may avoid seeking help altogether. Suicide prevention for neurodivergent populations requires not only availability of services but also care that affirms identity and adapts to diverse needs.
The Protective Role of Strengths and Community
Although risk factors are real and pressing, neurodiversity also brings strengths that can serve as protective factors against suicidal ideation. Many neurodivergent individuals describe intense passions, creativity, or problem-solving abilities that give life meaning. Communities built around shared neurodivergent identity provide belonging, advocacy, and mutual support.
Affirming these strengths and fostering environments of inclusion are critical components of prevention. When neurodivergent individuals are celebrated for who they are, rather than pathologized for their differences, suicide risk decreases.
What Suicide Prevention Must Address
Understanding how neurodiversity intersects with suicide risk requires a holistic approach. Prevention efforts must consider:
- Reducing stigma and increasing public awareness about neurodiversity.
- Expanding access to neurodiversity-affirming mental health care.
- Training clinicians to recognize and address suicide risk in neurodivergent populations.
- Supporting schools and workplaces in creating inclusive environments.
- Empowering neurodivergent voices in research, advocacy, and community leadership.
Prevention is not only about reducing risk but also about creating conditions where neurodivergent individuals can thrive.
Moving Forward
Suicide prevention cannot be one-size-fits-all. It must account for the realities of diverse populations, including the unique experiences of neurodivergent individuals. By acknowledging vulnerabilities, addressing systemic barriers, and affirming strengths, we can create pathways toward safety, belonging, and hope.
If you or someone you know is struggling with suicidal thoughts, immediate support is available through the 988 Suicide and Crisis Lifeline. For ongoing care, therapy can provide a safe and affirming space to explore identity, build coping strategies, and strengthen resilience.
At our practice, many of our associate therapists work with neurodivergent clients using affirming and compassionate approaches. We invite you to browse our therapist directory and connect with a provider who can support your journey with care that honors your full humanity.
FAQ: Neurodiversity and Suicide Prevention
How does recognizing neurodiversity change the way suicide prevention is approached?
Recognizing neurodiversity shifts suicide prevention away from a one-size-fits-all model toward an approach that honors the unique ways people experience and express distress. Rather than trying to make neurodivergent individuals fit into neurotypical frameworks, this perspective allows for care that is validating, individualized, and rooted in understanding. For example, interventions may focus on creating sensory-safe environments, using communication strategies that match the individual’s strengths, and affirming their identity rather than framing differences as deficits. This recognition helps people feel seen and respected, which is a critical protective factor against despair.
What role do families and caregivers play in supporting neurodivergent individuals at risk of suicide?
Families and caregivers are often the most consistent presence in a person’s life, and their support can be life-saving. They can create spaces of unconditional acceptance, advocate for accommodations in schools or workplaces, and model affirming language that reinforces self-worth. Caregivers also play an important role in noticing early changes in behavior or mood that may signal heightened distress. By educating themselves about neurodiversity, families can move beyond misunderstanding and criticism, replacing it with empathy, compassion, and strategies that empower their loved one to cope more effectively with challenges.
Are there cultural differences in how neurodiversity and suicide risk are understood?
Yes, cultural context shapes how both neurodivergence and suicide risk are perceived. In some communities, neurodivergent traits may be stigmatized or hidden, while in others certain traits such as strong memory, artistic creativity, or analytical skills may be celebrated. Cultural beliefs about mental health, help-seeking, and belonging strongly influence whether individuals feel safe accessing support. A therapeutic approach that integrates cultural humility recognizes these differences and encourages people to draw on the strengths of their cultural identity while addressing the unique barriers they may face.
How can schools and workplaces reduce suicide risk among neurodivergent people?
Schools and workplaces have the power to either deepen isolation or foster belonging. Institutions can reduce suicide risk by building inclusive cultures where neurodivergent individuals are accepted, valued, and supported. This can include offering sensory-friendly spaces, flexible scheduling, clear communication, and training for staff to better understand neurodiversity. When these environments acknowledge strengths, such as creativity, persistence, or innovation, individuals are more likely to thrive. Feeling respected and accommodated in these settings helps counteract the despair that can come from repeated experiences of rejection or misunderstanding.
How does intersectionality influence suicide risk for neurodivergent people?
Neurodivergent individuals do not experience their identities in isolation. A person who is both neurodivergent and part of another marginalized group may face compounded stigma. For example, a neurodivergent person of color might encounter both racism and ableism, while LGBTQ+ neurodivergent individuals may struggle against dual forms of exclusion. These overlapping experiences of discrimination can increase vulnerability to despair. Suicide prevention efforts that embrace intersectionality are more effective because they recognize the whole person, affirm multiple identities, and work to dismantle systemic barriers that create isolation.
Can technology and online communities help reduce suicide risk for neurodivergent populations?
Technology and online spaces can offer meaningful lifelines for neurodivergent individuals who may find in-person interactions overwhelming or inaccessible. Online communities can provide validation, shared identity, and support from peers who understand lived experiences. Therapy apps, text-based support, and moderated forums can also create safe and affirming avenues for help-seeking. Of course, these spaces require careful moderation to prevent harmful interactions, but when safe, they can become places of belonging and empowerment. For many neurodivergent individuals, these digital connections may feel more accessible and sustainable than traditional avenues of support.
What are the early warning signs of suicidal distress in neurodivergent individuals?
Warning signs can look different in neurodivergent individuals and may not always align with the patterns clinicians expect from neurotypical clients. Instead of withdrawing from social relationships, someone might disengage from their special interests or daily routines. Others may show an increase in meltdowns, irritability, or changes in sensory tolerance. Because communication styles differ, distress may be expressed through behaviors rather than words. Families, friends, and clinicians need to observe these shifts with curiosity and compassion, recognizing them as potential signals of internal struggle rather than dismissing them as “behavioral problems.”
How can clinicians adapt their practice to better support neurodivergent clients?
Clinicians can make a powerful difference by offering neurodiversity-affirming therapy that prioritizes respect, flexibility, and validation. This may involve adapting traditional talk therapy with visual tools, structured sessions, or slower pacing to match the client’s processing style. Building rapport often requires meeting clients where they are, including incorporating special interests into sessions as sources of strength and joy. Clinicians should avoid pathologizing neurodivergent traits, instead focusing on helping clients navigate distress, build coping strategies, and strengthen resilience. When clients feel both accepted and empowered, therapy can become a safe space where healing and hope are possible.