Reviewed by Kathryn Vercillo, MA Psychology | Last Updated: January 2026
What is Dialectical Behavior Therapy?
Dialectical Behavior Therapy (DBT) is an evidence based treatment that combines cognitive behavioral techniques with mindfulness practices and acceptance strategies. Originally developed for borderline personality disorder, DBT helps people who experience intense emotions develop skills for emotional regulation, distress tolerance, interpersonal effectiveness, and mindful awareness.

Finding Balance When Emotions Feel Overwhelming
Living with intense emotions can feel like riding a boat in perpetual storm. Small provocations trigger massive reactions. Relationships cycle through idealization and devastation. Self destructive impulses arise that rational thinking cannot override. You know your reactions are disproportionate, yet knowing does not stop them.
Dialectical Behavior Therapy offers a comprehensive approach for people who experience emotional intensity that disrupts their lives. Rather than simply managing symptoms, DBT teaches concrete skills that transform your relationship with emotion itself. Through structured learning and practice, you develop capacities for regulation that may have never fully developed or were overwhelmed by early experiences.
At Center for Mindful Therapy, some of our Associate Marriage and Family Therapists bring DBT training to clients throughout the San Francisco Bay Area. Some of our therapists offer in person sessions in San Francisco, Oakland, Berkeley, Marin, and other Bay Area communities, while telehealth options extend access across California. Whether you need individual therapy, skills group participation, or both, our trained clinicians can guide you through the DBT framework.
The therapy takes its name from the concept of dialectics, which involves holding opposing truths simultaneously. DBT balances acceptance of yourself as you are right now with commitment to change. It validates the difficulty of your experience while teaching you skills to respond differently. This both/and stance replaces the either/or thinking that often intensifies emotional suffering.
Our therapists work within a supervised model that ensures quality care while making DBT accessible. Each Associate MFT receives individual clinical supervision, bringing both current training in DBT protocols and the guidance of experienced clinicians to support your journey toward emotional balance. Note that our therapists all practice different modalities, so if you are looking specifically for a DBT therapist, make sure to check their profile and/or ask them in your initial call.
Browse our Therapist Directory
On This Page:
- Understanding DBT and Its Origins
- The Four DBT Skill Modules
- Components of DBT Treatment
- Conditions DBT Effectively Treats
- Core DBT Skills in Practice
- DBT Compared to Other Approaches
- Beginning Your DBT Journey
- Frequently Asked Questions
Understanding DBT and Its Origins
Marsha Linehan’s Revolutionary Approach
Marsha Linehan developed DBT in the 1980s while working with highly suicidal clients who were not responding to existing treatments. Standard cognitive behavioral therapy proved insufficient for people whose emotional reactivity was so intense that they could not engage with rational techniques during crisis.
Linehan recognized that these clients needed validation of their suffering alongside change strategies. Simply pushing for change communicated that something was wrong with them, intensifying shame and resistance. Yet pure acceptance without change left them trapped in destructive patterns. DBT emerged from synthesizing these seemingly contradictory needs.
Her personal disclosure that she had struggled with similar challenges earlier in life brought additional credibility to the approach. Linehan understood from inside what her clients experienced, informing a treatment that addresses emotional sensitivity with both scientific rigor and genuine compassion.
Research published in Frontiers in Psychology analyzing over 2,700 DBT studies from 1987 to 2024 reveals that interest in this approach has grown dramatically, particularly since 2015. The analysis found that DBT research has evolved from its original focus on borderline personality disorder and suicidal behavior to encompass studies on emotion dysregulation mechanisms and innovative digital interventions, reflecting the treatment’s expanding applications.
The Biosocial Model
DBT rests on a biosocial understanding of emotional dysregulation. Biological factors create emotional sensitivity: you may have been born with a nervous system that reacts more intensely to stimuli, returns to baseline more slowly, and has a lower threshold for activation. This biological vulnerability is not your fault; it is simply how your system is wired.
Social factors interact with this biology. When emotionally sensitive children grow up in invalidating environments, where their feelings are dismissed, punished, or treated as excessive, they do not learn adequate emotional regulation skills. Instead, they learn that their emotions are wrong, shameful, or too much. This invalidation can come from well meaning but misattuned caregivers, from traumatic experiences, or from cultural contexts that pathologize emotional expression.
The combination of biological vulnerability and invalidating environment creates pervasive emotional dysregulation. DBT addresses both sides: teaching skills that biological vulnerability made difficult to develop naturally, and providing validation that counters invalidating messages absorbed earlier.
What Dialectical Means
The word dialectical refers to integrating opposites rather than choosing between them. Instead of seeing yourself as either good or bad, either the victim or the problem, either needing to change or being acceptable as you are, dialectical thinking holds multiple truths simultaneously.
This both/and stance permeates DBT. Your therapist validates your pain while also expecting you to use skills. You accept yourself as you are while also committing to change. Your emotions make sense given your history while also creating problems that need addressing. Holding these apparent contradictions develops cognitive flexibility that reduces black and white thinking.
The primary dialectic in DBT is acceptance and change. Pure acceptance leaves you stuck. Pure change focus invalidates your struggle and often backfires. Synthesis involves accepting reality exactly as it is while also working to change it. This paradoxical stance proves remarkably effective.
Evidence Base and Research Support
DBT is among the most extensively researched psychotherapies. Dozens of randomized controlled trials demonstrate its effectiveness for borderline personality disorder, suicidal behavior, self harm, eating disorders, substance use, depression, and other conditions.
Research shows that DBT reduces suicidal behavior, self injury, psychiatric hospitalizations, treatment dropout, and depression severity. It improves social functioning, emotional regulation, and quality of life. These effects often maintain or continue improving after treatment ends.
A comprehensive review published in Behavior Therapy confirms that DBT has become established as a gold standard treatment for certain populations and behaviors, with dozens of randomized controlled trials demonstrating its effectiveness across populations and settings. The review emphasizes that while DBT has achieved significant validation, researchers continue working to improve access and efficacy across diverse communities.
The strong evidence base means that DBT is recommended as first line treatment for borderline personality disorder by clinical guidelines worldwide. It represents one of the most effective treatments available for people who have not responded to other approaches.
The Four DBT Skill Modules
DBT organizes skills training into four modules, each addressing different aspects of emotional and behavioral regulation. These modules work together, with skills from each area supporting and enhancing the others.
Mindfulness: The Foundation
Mindfulness forms the foundation of all DBT skills. The ability to observe your experience without immediately reacting, to notice thoughts as thoughts rather than facts, and to remain present even when emotions surge creates the platform from which all other skills operate.
DBT teaches specific mindfulness skills including observing, describing, and participating in your experience. You learn to notice thoughts, emotions, and sensations without judging them as good or bad. You practice being fully present in activities rather than running on autopilot or dissociating from experience.
The what skills describe what you do in mindfulness: observe, describe, and participate. The how skills describe how you do it: nonjudgmentally, one mindfully, and effectively. Together these create a framework for engaging with experience that reduces automatic reactivity.
Mindfulness in DBT has practical purpose rather than spiritual orientation. Whether or not you have interest in meditation traditions, these skills help you respond rather than react, notice choices where automatic patterns previously operated, and stay present enough to use other skills when needed.
Distress Tolerance: Surviving Crisis Without Making It Worse
When emotions peak beyond the point where other skills help, distress tolerance skills prevent destructive behavior. These skills are not about feeling better but about getting through intense moments without making your situation worse through impulsive action.
Crisis survival skills include distraction techniques like ACCEPTS (Activities, Contributing, Comparisons, Emotions, Pushing away, Thoughts, Sensations), self soothing through the five senses, and improving the moment through strategies like imagery, meaning, prayer, relaxation, one thing in the moment, vacation, and encouragement (IMPROVE).
The TIPP skills offer rapid physiological intervention: Temperature (cold water on face triggers the dive reflex, slowing heart rate), Intense exercise (burns off adrenaline), Paced breathing (activates parasympathetic nervous system), and Paired muscle relaxation. These body based techniques provide relief when cognitive strategies cannot yet be accessed.
Radical acceptance, a core distress tolerance skill, involves fully accepting reality exactly as it is rather than fighting against facts you cannot change. This acceptance does not mean approval or passive resignation but rather ending the suffering added by refusing to accept what has already happened. Pain is inevitable; suffering from fighting reality is optional.
Emotion Regulation: Understanding and Influencing Emotions
Emotion regulation skills help you understand emotional experiences, reduce vulnerability to intense emotions, and change unwanted emotional responses. Rather than being controlled by feelings, you develop capacity to influence your emotional life.
Understanding emotions involves recognizing the function emotions serve, identifying and naming what you feel, and distinguishing between primary emotions (the first reaction) and secondary emotions (reactions to your reactions). This clarity reduces the chaos of being flooded by unnamed experience.
Reducing vulnerability involves attending to physical factors that affect emotional resilience. PLEASE skills address PhysicaL illness, balanced Eating, avoiding mood Altering substances, balanced Sleep, and Exercise. When your body is compromised, emotional regulation becomes much harder. Self care is not indulgent but necessary for emotional stability.
Changing emotions involves strategies like opposite action (doing the opposite of what the emotion urges when the emotion does not fit the facts or acting on it is not effective), problem solving (when the emotion fits the situation), and checking the facts (ensuring your interpretation is accurate before reacting).
Building positive experiences, both in the short term and long term, increases positive emotions and builds resilience. This involves both engaging in pleasant activities and working toward values driven goals that provide meaning and satisfaction.
Interpersonal Effectiveness: Navigating Relationships Skillfully
Interpersonal effectiveness skills help you navigate relationships while maintaining self respect, achieving your objectives, and preserving the relationship. Many people struggle with these competing priorities, sacrificing their needs to maintain connection or damaging relationships by pursuing goals without regard for the other person.
DEAR MAN provides a framework for asking for what you want or saying no effectively: Describe the situation objectively, Express your feelings, Assert what you want clearly, Reinforce by explaining benefits for the other person, stay Mindful of your objective, Appear confident, and Negotiate if needed.
GIVE skills focus on maintaining the relationship: be Gentle, act Interested, Validate the other person’s perspective, and use an Easy manner. These skills matter when relationship preservation is your primary goal.
FAST skills maintain self respect: be Fair to yourself and the other person, avoid unnecessary Apologies, Stick to your values, and be Truthful. These skills prevent self abandonment in pursuit of connection.
The interpersonal effectiveness module also teaches how to evaluate whether relationships are healthy, how to end destructive relationships, and how to build new connections. For people whose emotional intensity has complicated relationships, these skills provide practical guidance.
Components of DBT Treatment
Standard comprehensive DBT includes multiple components that work together. While some clients engage with individual elements, the full program provides the most robust treatment.
Individual Therapy
Individual DBT sessions occur weekly and focus on applying skills to your specific life situations. Your therapist helps you understand your patterns, problem solve around current challenges, and process distressing experiences using DBT framework.
Sessions use diary cards that track target behaviors, emotions, and skill use between sessions. This tracking provides data about patterns and progress while keeping treatment focused on behavioral change rather than abstract discussion.
Your individual therapist uses a hierarchy of treatment targets. Decreasing life threatening behaviors takes priority, followed by therapy interfering behaviors, then quality of life interfering behaviors. This structure ensures that the most serious concerns receive attention first.
The individual therapy relationship itself provides validation and models dialectical thinking. Your therapist balances empathy for your struggles with expectation that you use skills. They validate your emotions while also gently challenging avoidance and pushing toward change.
Skills Training Group
Skills groups meet weekly for approximately two hours, usually over about six months to complete all four modules, though many programs cycle through modules repeatedly. Groups follow a structured curriculum, teaching skills systematically and providing homework for between session practice.
The group format offers several advantages. You learn that others share your struggles, reducing shame and isolation. It offers the opportunity to practice interpersonal effectiveness skills in real time. You learn from others’ questions and applications. The educational structure provides coverage of material that individual therapy alone might not address as systematically.
Groups are not process groups focused on sharing personal experiences but psychoeducational classes focused on skill acquisition. While support naturally develops among members, the primary purpose is learning and practicing skills.
Research published in Behavior Therapy notes that skills training has emerged as a particularly valuable component, with studies showing that even standalone DBT skills groups can produce meaningful improvements for people who cannot access comprehensive treatment.
Bay Area residents benefit from the variety of group options available. Some therapists in our collective offer DBT skills groups at different times and locations, increasing accessibility.
Phone Coaching
Between sessions, clients can contact their individual therapist briefly for coaching in applying skills to real time situations. This coaching helps bridge the gap between learning skills in calm settings and using them during actual crises.
Phone coaching follows specific guidelines. Calls are brief, focused on skill application, and occur before engaging in problem behaviors rather than afterward. The purpose is teaching you to reach out for help and apply skills in the moment, not to provide extended support between sessions.
This component addresses a common problem: knowing what to do but being unable to access that knowledge during crisis. Brief coaching can help you identify what skill might help and how to apply it right now, in this situation.
Consultation Team
DBT therapists meet regularly as a consultation team to support each other in providing effective treatment. Treating emotionally dysregulated clients can be challenging, and the team structure prevents burnout and maintains treatment fidelity.
While clients do not participate in consultation team meetings, knowing that your therapist receives support and accountability benefits your treatment. The team helps therapists maintain the delicate balance of validation and change, avoid common pitfalls, and manage their own reactions to challenging therapeutic moments.
Conditions DBT Effectively Treats
While developed for borderline personality disorder, DBT has proven effective for multiple conditions involving emotional dysregulation. The following areas respond particularly well to this structured approach.
Borderline Personality Disorder
DBT remains the treatment of choice for borderline personality disorder, the condition for which it was developed. BPD involves unstable relationships, identity disturbance, impulsivity, emotional instability, chronic emptiness, anger problems, and often self harm or suicidal behavior.
Research demonstrates that DBT significantly reduces suicidal behavior, self injury, hospitalizations, and treatment dropout in people with BPD. It improves emotional regulation, reduces depression and anxiety, and enhances social functioning. These gains often maintain after treatment ends.
Bay Area residents struggling with BPD find that DBT provides practical tools that other approaches lacked. The validation component addresses the shame and self hatred common in BPD while the skills training provides concrete strategies for managing symptoms.
The structured nature of DBT helps where other treatments failed. Clear expectations, diary cards, hierarchy of targets, and skills curriculum provide containment that unstructured therapy often cannot offer for BPD. The team approach prevents the splitting dynamics that frequently disrupt treatment.
Self Harm and Suicidal Behavior
DBT was specifically designed to address self harm and suicidal behavior, and these remain its strongest applications. The treatment directly targets these behaviors as highest priority while building skills that address the underlying dysregulation driving them.
Crisis survival skills provide alternatives to self harm when distress peaks. Distress tolerance skills help you survive intense moments without acting destructively. Emotion regulation skills reduce the frequency and intensity of emotional states that prompt self harm urges.
The non judgmental stance of DBT reduces shame around self harm, allowing honest discussion and problem solving. Your therapist treats self harm as a behavior serving a function (typically emotion regulation) rather than as manipulation or attention seeking. This understanding informs skill building that addresses the function self harm has served.
A study published in The Journal of the American Academy of Psychiatry and the Law found that patients participating in DBT showed significant reductions in assaultive incidents and decreased reliance on emergency medications over the course of treatment. Participants also demonstrated meaningful improvements in depression symptoms, psychological flexibility, and coping skills within the first six months, supporting DBT’s effectiveness for behavioral and emotional regulation challenges.
Eating Disorders
DBT has been adapted effectively for eating disorders including binge eating disorder, bulimia nervosa, and anorexia nervosa. Eating disorder behaviors often serve emotional regulation functions similar to self harm: numbing painful feelings, providing sense of control, or punishing the self.
Emotion regulation skills address the dysregulation underlying disordered eating. Distress tolerance skills provide alternatives to bingeing, purging, or restricting when urges arise. Mindful eating skills help rebuild healthy relationships with food and body signals.
The validation component proves particularly valuable for eating disorders, which often involve profound shame and harsh self judgment. DBT’s acceptance stance helps clients develop compassion for themselves while also committing to behavioral change.
Substance Use Disorders
DBT for substance use disorders helps people develop skills for managing urges, tolerating distress without substances, and building lives worth living that do not require numbing. The approach addresses emotional dysregulation that often underlies addiction.
Distress tolerance skills provide alternatives when cravings or emotional pain trigger urges to use. Mindfulness skills help observe urges without acting on them. Emotion regulation skills reduce the intensity of states that prompt substance use.
DBT’s acceptance orientation fits well with addiction treatment. Validating the difficulty of recovery while expecting behavioral change mirrors the approach of many recovery programs. Skills training provides concrete tools that complement other addiction supports.
Depression and Anxiety
While not first line treatments for uncomplicated depression or anxiety, DBT offers significant benefits when these conditions co occur with emotional dysregulation or have not responded to other approaches.
Emotion regulation skills directly address depressive symptoms through behavioral activation, opposite action, and building mastery. The structure of skills training and diary cards provides accountability that can be particularly helpful when depression undermines motivation.
For anxiety, mindfulness skills help observe anxious thoughts without fusion. Distress tolerance skills manage anxiety peaks. The emphasis on accepting reality reduces the additional suffering caused by resisting what is already true.
Complex PTSD and Trauma
DBT’s emphasis on emotional regulation makes it valuable for complex trauma where dysregulation is prominent. While not specifically a trauma treatment, DBT provides stabilization and skills that support subsequent or concurrent trauma processing.
Many clinicians use DBT as a first phase treatment for complex PTSD, building skills before engaging in trauma focused approaches like EMDR or prolonged exposure. The distress tolerance skills prove especially valuable when trauma processing activates intense states.
DBT’s validation of suffering without requiring detailed trauma narrative feels safer to some trauma survivors than approaches emphasizing exposure. Skills can be built without repeatedly discussing traumatic material.
Mood Instability and Bipolar Disorder
While medication typically forms the foundation of bipolar treatment, DBT provides valuable adjunctive support for the emotional dysregulation and interpersonal difficulties that often accompany bipolar disorder.
Skills help manage mood episodes, recognize early warning signs, and maintain medication adherence. The structure and psychoeducation help clients understand their condition and develop self management strategies.
Core DBT Skills in Practice
Understanding key skills in more detail illustrates how DBT works practically. These selected skills represent the approach and provide immediate utility.
Wise Mind
Wise Mind refers to the synthesis of Emotion Mind (when emotions drive thinking and behavior) and Reasonable Mind (when logic dominates without regard for emotion). Most people vacillate between these states, acting from emotion then overcorrecting into cold logic.
Wise Mind integrates both, accessing emotional information while also thinking clearly. From Wise Mind, you can honor what you feel while also considering consequences and effectiveness. Decisions from Wise Mind tend to align with your values rather than impulsive reactions or disconnected analysis.
Accessing Wise Mind involves pausing to notice which mind is currently dominant, then using mindfulness to find the synthesis. Practices like asking what Wise Mind would say about a situation or imagining dropping down into Wise Mind help develop this capacity.
Radical Acceptance
Radical acceptance means fully accepting reality exactly as it is, without judgment, resistance, or attempts to change what cannot be changed. This acceptance extends to yourself, others, events, and life as a whole.
Radical acceptance does not mean approval, agreement, or giving up on change. You can radically accept that something happened while also working to prevent its recurrence. You can accept current circumstances while also changing them going forward. The acceptance is of reality in this moment, not of all futures.
Refusing to accept reality adds suffering beyond the pain of the reality itself. When you mentally fight against what has already occurred, you create additional distress that compounds your struggles. Radical acceptance ends this additional suffering by allowing reality to be exactly what it is.
STOP Skill
STOP provides an in the moment intervention for preventing impulsive behavior. When emotions surge and urges arise, STOP interrupts the automatic sequence.
Stop: Freeze, do not act. Put your hands in your pockets if needed. Take a step back: Remove yourself from the situation if possible. Take a breath. Observe: Notice what is happening inside and outside you. Proceed mindfully: Consider your options and choose based on what is effective.
This brief pause can prevent actions you would regret. The intensity of the urge often diminishes in the time STOP creates. Even a few seconds can access enough Wise Mind to make better choices.
Opposite Action
Opposite action involves acting contrary to what an emotion urges when that emotion does not fit the facts or when acting on the urge would be ineffective. By changing the action, you influence the emotion itself.
Fear urges escape, so opposite action involves approaching what you fear (when it is not actually dangerous). Sadness urges withdrawal, so opposite action involves getting active and engaging. Anger urges attacking, so opposite action involves gentle avoidance or kindness. Shame urges hiding, so opposite action involves sharing your experience with supportive others.
For opposite action to work, it must be complete: all the way opposite, with committed body language and facial expression, not half hearted or resentful. The body’s experience of opposite action sends signals to the brain that help shift the emotion.
PLEASE Skills
PLEASE skills reduce emotional vulnerability through physical self care. When your body is compromised, emotional regulation becomes exponentially harder. These skills address preventable physical factors.
Treat PhysicaL illness: See doctors, take prescribed medications, manage chronic conditions. Balance Eating: Eat regularly, not too much or too little, with reasonable nutrition. Avoid mood Altering substances: Limit alcohol and drugs that destabilize mood. Balance Sleep: Get adequate sleep, maintain consistent sleep schedule. Exercise: Move your body regularly in ways that work for you.
These basics often get neglected when emotions overwhelm. Yet attending to them provides foundation for all other skills. You cannot expect emotional stability on inadequate sleep, poor nutrition, and no exercise.
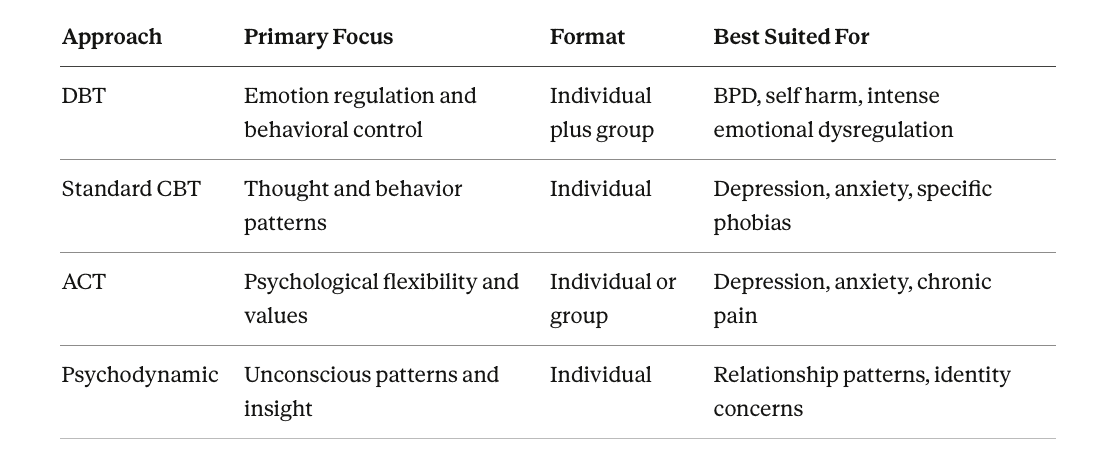
DBT Compared to Other Approaches
Standard Cognitive Behavioral Therapy and DBT
DBT emerged from CBT and shares its emphasis on identifying and changing problematic thought and behavior patterns. Both approaches are structured, goal oriented, and emphasize skill building.
DBT differs in several key ways. The validation component and acceptance strategies balance the change focus of standard CBT. Mindfulness forms a core component rather than an occasional addition. The explicit focus on emotion regulation addresses a dimension that standard CBT can neglect. The multiple components (individual, group, phone coaching, consultation team) provide more intensive support.
For people whose emotional intensity prevents engagement with standard CBT techniques, DBT provides the validation and distress tolerance skills needed to access cognitive strategies. DBT can serve as a platform that enables CBT to be effective.
DBT and Psychodynamic Therapy
Psychodynamic therapy emphasizes understanding unconscious patterns and historical origins of current difficulties. Insight develops through exploring the therapeutic relationship, dreams, early memories, and current patterns.
DBT differs in its explicit focus on behavioral change and skill building. While understanding can develop, the primary mechanism of change is acquiring and using new capabilities rather than developing insight. The structured approach contrasts with the more exploratory nature of psychodynamic work.
For some clients, the combination proves valuable: DBT provides skill building and behavioral control while psychodynamic work addresses deeper patterns and historical material. Sequencing DBT before insight oriented work makes sense when behavioral instability would prevent engaging in less structured therapy.
DBT and Other Skills Based Approaches
Several treatments share DBT’s emphasis on skill building, including Acceptance and Commitment Therapy (ACT) and Mentalization Based Treatment (MBT). Each has distinct emphases while sharing the general approach of building specific capabilities.
ACT focuses on psychological flexibility, values clarification, and accepting internal experiences while committing to behavior change. DBT has more specific skill protocols and more explicit focus on emotion regulation.
MBT emphasizes developing capacity to understand mental states in self and others, particularly valuable for the interpersonal instability in borderline presentations. DBT has broader skill focus beyond mentalization specifically.
The choice between these approaches depends on specific presentation, treatment availability, and client preference. All have evidence support for overlapping populations.
Beginning Your DBT Journey
Finding DBT Treatment
Our therapist directory allows you to search for clinicians with DBT training. Some therapists offer comprehensive DBT including both individual therapy and skills groups. Others provide DBT informed individual therapy or lead skills groups that clients attend alongside individual therapy with different providers.
When contacting potential therapists, ask about their DBT training and what components they offer. Have they completed intensive DBT training? Do they offer or have access to skills groups? Do they provide phone coaching? Understanding what is available helps you find appropriate treatment.
For full DBT, you may need to piece together components: one therapist for individual sessions, another provider for skills group. Your individual therapist can help coordinate this arrangement.
Assessment and Getting Started
Treatment begins with assessment to determine if DBT is appropriate for your situation. Your therapist evaluates your symptoms, history, current functioning, and treatment goals. Together you discuss what DBT involves and whether commitment to this structured approach feels workable.
If DBT is appropriate, you develop explicit treatment targets and establish agreements about attendance, diary card completion, and phone coaching parameters. These clear expectations create structure that supports the work. Orientation includes education about the biosocial model, the treatment components, and what DBT asks of you.
Initial sessions focus on beginning to establish the therapeutic relationship. Your therapist learns about your history, symptoms, and goals. You learn about DBT structure and begin discussing treatment targets. If joining a skills group, early group sessions orient you to format and begin the mindfulness module.
Diary cards begin immediately, building the habit of tracking before crisis situations arise. Early tracking provides baseline data and familiarizes you with the format.
Commitment and Expectations
DBT asks significant commitment. Weekly individual therapy, weekly skills group, diary card completion, homework practice, and availability for phone coaching require substantial time and engagement. Before beginning, honestly assess whether you can make this commitment.
The structure serves purpose. Emotional dysregulation does not improve through occasional contact and passive participation. The frequency and accountability build skills through repetition and application. Commitment to the structure predicts outcomes.
Discuss expectations explicitly with your therapist. What happens if you miss sessions? How should you use phone coaching? What are consequences for incomplete diary cards? Clear agreements prevent misunderstandings and support the work.
The Treatment Process
Standard DBT progresses through phases. The first phase focuses on gaining control over life threatening and treatment interfering behaviors. If you engage in self harm, suicidal behavior, or other dangerous actions, these become primary targets. Diary cards track urges and behaviors, and individual therapy sessions conduct behavioral chain analysis to understand what led to problematic behaviors.
Simultaneously, you begin skills group, learning and practicing the four modules. Skills acquired in group get applied to current situations in individual therapy. As behavioral control stabilizes, treatment expands focus to quality of life issues: relationship improvement, career development, processing past experiences, or building a life worth living.
Many clients cycle through the skills modules multiple times, deepening understanding with each pass. Repetition builds the automaticity needed for skills to be accessible during actual difficult moments.
Duration and Building Your Support Team
Standard comprehensive DBT typically lasts about one year, though duration varies based on presenting concerns and individual progress. This allows time to cycle through all four skill modules while also addressing individual treatment targets.
Full DBT treatment involves a team: individual therapist, skills group leader, and other clients in your group. Building these relationships and learning to use phone coaching establishes the support structure for the work ahead.
The skills group creates community with others who share your struggles. While not a process group, the shared experience of learning and practicing skills builds connection and reduces isolation. Many clients find that group membership itself provides significant benefit.
After completing intensive DBT, many clients step down to maintenance level support: individual therapy without group, periodic check ins, or brief returns to skills group for refresher. Graduation from intensive treatment marks an achievement, not abandonment.
For questions about DBT or assistance finding appropriate treatment in the Bay Area, contact us.
Browse our Therapist Directory
Frequently Asked Questions About DBT
Q: Do I need to have borderline personality disorder to benefit from DBT?
A: No. While DBT was developed for borderline personality disorder and has the strongest evidence for that condition, it has proven effective for many other issues involving emotional dysregulation. If you experience intense emotions that disrupt your life, difficulty managing distress, impulsive behaviors you regret, or unstable relationships connected to emotional intensity, DBT may help regardless of your specific diagnosis.
DBT has been successfully adapted for eating disorders, substance use disorders, depression, anxiety, self harm without BPD diagnosis, and emotion dysregulation from various causes. The core skills help anyone who struggles with intense emotions and their consequences.
That said, DBT is an intensive treatment with significant time commitment. For milder difficulties, briefer or less intensive approaches may suffice. Your therapist can help you assess whether full DBT is warranted or whether DBT informed work or other approaches might serve you better.
Q: What is the difference between DBT skills group and group therapy?
A: DBT skills group is a structured psychoeducational class focused on teaching and practicing specific skills. Groups follow a curriculum, assign homework, and prioritize skill acquisition. While support naturally develops among members and brief personal sharing occurs, the primary focus is learning material rather than processing personal experiences.
Traditional group therapy involves members sharing experiences, receiving feedback, and processing interpersonal dynamics within the group. The group relationships and interactions become the focus of therapeutic work.
In DBT, the skills group teaches the curriculum while individual therapy addresses personal application and processing. This separation allows groups to cover material efficiently without getting sidetracked into individual processing that would shortchange skill instruction.
Q: How long does DBT treatment typically last?
A: Standard comprehensive DBT typically lasts about one year. This allows time to cycle through all four skill modules at least once while also addressing individual treatment targets in individual therapy. Many clients benefit from cycling through modules multiple times, deepening skill acquisition with each pass.
Treatment length varies based on presenting concerns, progress, and individual needs. Some clients achieve goals faster, while others with more complex presentations benefit from extended treatment. The one year framework provides structure while allowing flexibility.
After completing intensive DBT, many clients step down to maintenance level support rather than stopping abruptly. This might involve continued individual therapy without group, periodic check ins, or brief returns to skills group for refresher. Graduation from intensive treatment marks an achievement, not abandonment.
Q: Can I do DBT through telehealth, or do I need to attend in person?
A: Both individual DBT and skills groups can be delivered effectively through telehealth. Research during and after the pandemic demonstrated that video delivery maintains effectiveness for most clients. Telehealth expands access significantly, allowing you to work with DBT trained therapists regardless of geographic distance.
Some clients prefer in person treatment for the increased sense of connection and presence. Others appreciate the convenience and accessibility of telehealth. Our therapists throughout the Bay Area offer various formats, and many provide both in person and video options.
Phone coaching works the same whether your other treatment is in person or telehealth. Brief skill coaching calls support real time application regardless of how you attend sessions.
Q: What if I have trouble with the group component? Can I just do individual DBT?
A: While comprehensive DBT includes both individual therapy and skills group, some clients cannot access or participate in groups due to scheduling, social anxiety, or other factors. Individual DBT without group is less complete but can still provide significant benefit.
When skills group is not possible, individual therapy takes more responsibility for skill teaching that would otherwise happen in group. Your therapist spends session time on psychoeducation and skill practice that group would otherwise cover. This adaptation works but requires more individual session time for comparable skill acquisition.
If social anxiety makes group feel impossible, this itself becomes a treatment target. DBT skills help manage the anxiety while the group provides gradual exposure to social situation. Many socially anxious clients find DBT groups less threatening than other group formats because of the structured, educational nature.
If you strongly prefer avoiding group, discuss this with your therapist. Together you can determine whether individual only treatment could meet your needs or whether addressing the group resistance should become part of the work.
Q: Is DBT compatible with medication?
A: Yes. DBT frequently occurs alongside psychiatric medication and views medication as potentially valuable adjunct rather than competing approach. Many clients with the conditions DBT treats benefit from medication for mood stabilization, anxiety reduction, or other purposes.
DBT therapists coordinate with prescribers when clients take psychiatric medication. The behavioral focus of DBT complements the biological focus of medication. Skills help with what medication cannot directly address while medication provides foundation that makes skill use possible.
Decisions about medication remain between you and your prescriber. DBT therapists do not prescribe or recommend specific medications but do encourage clients to work with qualified prescribers when medication might help and to take prescribed medications as directed.
Q: What if I have tried DBT before and it did not help?
A: Several factors affect DBT outcomes, and previous unsuccessful attempts do not necessarily predict future results. Consider what might have been different about previous treatment.
Did you receive comprehensive DBT with all components, or DBT informed treatment with some elements missing? Full DBT requires individual therapy, skills group, phone coaching availability, and therapist consultation team. Missing components reduce effectiveness.
Were you able to fully commit to the treatment at that time? DBT requires significant engagement. If life circumstances, ambivalence, or other factors prevented full participation, outcomes would be affected.
Did the therapist fit feel right? Therapeutic relationship matters even in structured treatments like DBT. A different therapist might create different conditions for success.
What has changed since then? You may have developed readiness, insight, or circumstances that make the work more accessible now. Previous treatment, even if seemingly unsuccessful, may have planted seeds that make current treatment more effective.
Discussing your previous DBT experience with potential therapists helps them understand what to do differently and helps you assess whether trying again makes sense.
Related Therapy Services
- ACT Therapy: Acceptance and Commitment Therapy shares DBT’s acceptance orientation while emphasizing values driven living and psychological flexibility.
- Cognitive Behavioral Therapy: The parent approach from which DBT emerged, effective for depression, anxiety, and specific behavioral concerns.
- Trauma Therapy: For clients whose emotional dysregulation connects to trauma, trauma focused approaches complement DBT stabilization work.
- Mindfulness Based Therapies: Approaches that deepen the mindfulness component central to DBT.
Citations:
- Rizvi, S. L., Bitran, A. M., Oshin, L. A., Yin, Q., & Ruork, A. K. (2024). The state of the science: Dialectical behavior therapy. Behavior Therapy, 55(6), 1233-1248. https://doi.org/10.1016/j.beth.2024.02.006
- Shi, K., Zhang, L. Y., Gao, B. L., Qian, Y., Huang, X. B., & Yue, J. L. (2025). Bibliometric analysis of global research on dialectical behavior therapy from 1987 to 2024. Frontiers in Psychology, 16, 1450497. https://doi.org/10.3389/fpsyg.2025.1450497
- Marshall, L., Kletzka, N., Kanitz, J., Opperman, K. J., & Rockwell, J. (2024). Effectiveness of dialectical behavior therapy (DBT) in a forensic psychiatric hospital. Journal of the American Academy of Psychiatry and the Law, 52(2). https://doi.org/10.29158/JAAPL.240009-24